
INFOGRAPHICS: “COVID-19 COMPARED TO OTHER DISEASES AND CONDITIONS”


Dr. Sachin Nagrani, Medical Director at HEAL, talks about the benefits and growth in Telemedicine appointments.
From Harvard Medical School (June 4, 2020):
“We took an unbiased approach and searched throughout the body for indicators of damage from sleep deprivation. We were surprised to find it was the gut that plays a key role in causing death,” said senior study author Dragana Rogulja, assistant professor of neurobiology in the Blavatnik Institute at HMS.
The first signs of insufficient sleep are universally familiar. There’s tiredness and fatigue, difficulty concentrating, perhaps irritability or even tired giggles. Far fewer people have experienced the effects of prolonged sleep deprivation, including disorientation, paranoia, and hallucinations.

Total, prolonged sleep deprivation, however, can be fatal. While it has been reported in humans only anecdotally, a widely cited study in rats conducted by Chicago-based researchers in 1989 showed that a total lack of sleep inevitably leads to death. Yet, despite decades of study, a central question has remained unsolved: Why do animals die when they don’t sleep?
Now, Harvard Medical School (HMS) neuroscientists have identified an unexpected, causal link between sleep deprivation and premature death.
From The Lancet Diabetes & Endocrinology (June 2020):
Our findings show that the intensive lifestyle intervention led to significant weight loss at 12 months, and was associated with diabetes remission in over 60% of participants and normoglycaemia in over 30% of participants. The provision of this lifestyle intervention could allow a large proportion of young individuals with early diabetes to achieve improvements in key cardiometabolic outcomes, with potential long-term benefits for health and wellbeing.

Type 2 diabetes is affecting people at an increasingly younger age, particularly in the Middle East and in north Africa. We aimed to assess whether an intensive lifestyle intervention would lead to significant weight loss and improved glycaemia in young individuals with early diabetes..Between July 16, 2017, and Sept 30, 2018, we enrolled and randomly assigned 158 participants (n=79 in each group) to the study. 147 participants (70 in the intervention group and 77 in the control group) were included in the final intention-to-treat analysis population. Between baseline and 12 months, the mean bodyweight of participants in the intervention group reduced by 11·98 kg (95% CI 9·72 to 14·23) compared with 3·98 kg (2·78 to 5·18) in the control group (adjusted mean difference −6·08 kg [95% CI −8·37 to −3·79], p<0·0001). In the intervention group, 21% of participants achieved more than 15% weight loss between baseline and 12 months compared with 1% of participants in the control group (p<0·0001). Diabetes remission occurred in 61% of participants in the intervention group compared with 12% of those in the control group (odds ratio [OR] 12·03 [95% CI 5·17 to 28·03], p<0·0001). 33% of participants in the intervention group had normoglycaemia compared with 4% of participants in the control group (OR 12·07 [3·43 to 42·45], p<0·0001)
In this audio interview conducted on June 3, 2020, the editors discuss two new studies: one comparing test swabs collected by health care workers with swabs collected by the patients themselves and one assessing hydroxychloroquine treatment in people who had been exposed to Covid-19 but weren’t yet ill.
The continuing spread of SARS-CoV-2 remains a Public Health Emergency of International Concern. What physicians need to know about transmission, diagnosis, and treatment of Covid-19 is the subject of ongoing updates from infectious disease experts at the Journal.
Eric Rubin is the Editor-in-Chief of the Journal. Lindsey Baden is a Deputy Editor of the Journal. Stephen Morrissey, the interviewer, is the Executive Managing Editor of the Journal.

COMMENTARY
The technology of telemedicine will predictably and steadily get better.
Medical assistants, mostly human at present, are commonplace, notably in specialty offices, and machines using improving voice-to-text transcription are getting better.
Wearable devices are proliferating and hopefully coming down in cost, and platform technology is improving though still glitchy.
Patients generally accept Telemedicine. They like the saving of travel time and infection exposure.
Doctors may drag their feet because the increased effort and legal exposure is not compensated by increase in payment. On the contrary, pre-Covid compensation was LESS for a televisit. Continuing Parity would help.
The politicians at the state level should eventually make licenses valid across state borders.
The big wild card is the Legal Profession. Unless they develop restraint( and litigious patients reform), there could be a feeding Frenzy, which would delay implementation of a very good idea.
Eventually telemedicine deserves to be 50% or more of medical practice.
From the Wall Street Journal (June 1, 2020):
“The biggest problem has been staying asleep,” says Philip Muskin, a professor of psychiatry at Columbia University Medical Center in New York. “People aren’t exercising, their days have no structure at all.”

Preliminary results from a survey taken by around 1,600 people from 60 countries show that 46% reported poor sleep during the pandemic, while only 25% said they had slept poorly before it, according to Melinda Jackson, a senior lecturer at the Turner Institute for Brain and Mental Health at Monash University in Melbourne, who studies how stressful events affect people’s sleep. Forty percent also reported increased alcohol consumption.
The key is to prevent the sleep problem from becoming chronic, she says. It is important to avoid associating your bed or bedroom with a place where you are awake. Experts recommend that if you can’t fall asleep, or wake up in the middle of the night and are unable to go back to sleep after 20 minutes, get out of bed and do something relaxing.
I should have known something was wrong.
I was getting short of breath with a third of a 45-minute exercise I had done for years, but I rationalized it away. I reasoned that I hadn’t been sleeping well, I am getting old. And my heart isn’t working as well because of the Atrial Fibrillation.
Physicians have a big armamentarium of excuses they can generate, and besides it is their Karma to GIVE Medical care rather than to RECEIVE it.
The AHA moment came when I bumped my leg, and peeled back some skin. My skin is old and fragile, and I’m always tearing it in small areas.
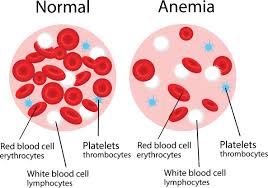
This time, I got to see the blood run all the way down my leg like a drop of grape juice, not the thick blood I’m used to. If anything, my blood should be thicker, more viscous, since my average Hemoglobin is 16 gm., on the high side of normal.
I got my blood drawn, and ordered a CBC and a ferritin. The CBC shows the Hemoglobin level, and a number of other measurements bearing on anemia, and the ferritin gives a measure of IRON STORES.
I can’t remember the first time my ferritin was ordered, or why, but it has for years been borderline, just barely in the normal range, dipping down as low as 18, and rising as high as 35.
Since a common cause of low iron stores with a good diet is colon cancer, I had about 3 colonoscopies to rule out cancer over a period of 6 years; lucky me.
At least they were all negative, and without polyps.
This time the ferritin was 12, well into the abnormal range, and the Hemoglobin was 8.6 gm. little more than half my usual.
I had been fibrillating for 5 months, and been on 5 mg. Eliquis ( an anticoagulant/blood thinner) for the same period. Having a recent normal colonoscopy, the most likely diagnosis was AVMs (arteriovenous malformations) of the small bowel, with bleeding accelerated by the Eliquis,
Since small bowel surgery contraindicated a diagnostic videocapsule, this diagnosis would have to remain an assumption.
I reduced the Eliquis by 25%, calculated my blood loss rate and started 2 capsules of feosol alternating with 3 capsules daily. Over a period of 4 months, my Hemoglobin came back up to 15 gm., and my ferritin came up to 50. I am due another test as soon as I get enough nerve to brave the Covid and go to the lab.
This story is a good illustration of treating one illness, and thereby creating another in this world awash with medication. How much better it is to stay as healthy as possible.
However, I am becoming increasingly aware of the fact that Health is not often the top priority in most peoples lives.
As an illustration, I refer to todays’ Sunday New York Times, which reviewed 2 books on walking, one written to praise its’ health benefits. To quote the reviewer, “
The issue with ‘ in praise of walking’ is Mr. O’Mara’s assumption that how good an activity may be for us is the most essential measure of its worth”. Praising health raises an issue?
Personally, my main exercise is walking, and I do it expressly for health. That doesn’t mean that I don”t enjoy walking and have other motivations. I would not be walking as FAST, however, it it were not so healthy.
From the New York Times
….in the case of the new coronavirus, people who have no symptoms seem to have viral loads — that is, the amount of virus in their bodies — just as high as those who are seriously ill, according to some studies.

When experts recommend wearing masks, staying at least six feet away from others, washing your hands frequently and avoiding crowded spaces, what they’re really saying is: Try to minimize the amount of virus you encounter.
A few viral particles cannot make you sick — the immune system would vanquish the intruders before they could. But how much virus is needed for an infection to take root? What is the minimum effective dose?
And coronavirus patients are most infectious two to three days before symptoms begin, less so after the illness really hits.
Some people are generous transmitters of the coronavirus; others are stingy. So-called super-spreaders seem to be particularly gifted in transmitting it, although it’s unclear whether that’s because of their biology or their behavior.
On the receiving end, the shape of a person’s nostrils and the amount of nose hair and mucus present — as well as the distribution of certain cellular receptors in the airway that the virus needs to latch on to — can all influence how much virus it takes to become infected.
COMMENTARY