In this episode of the Heart podcast, Digital Media Editor, Dr James Rudd, is joined by Professor Carolyn Lam, a world expert in heart failure from the University of Singapore and the National Heart Centre, also in Singapore.
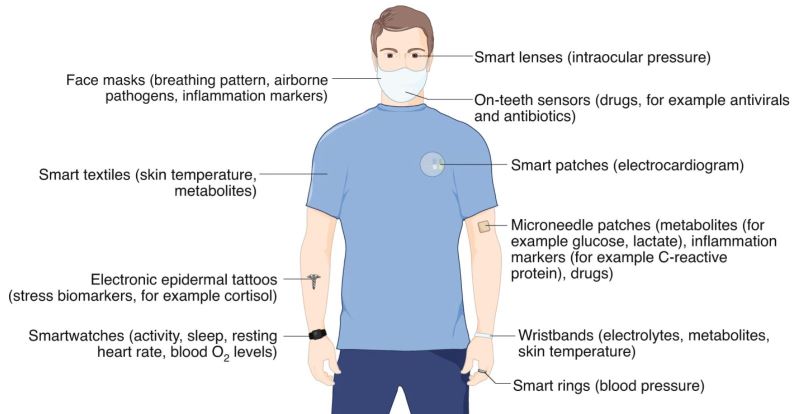
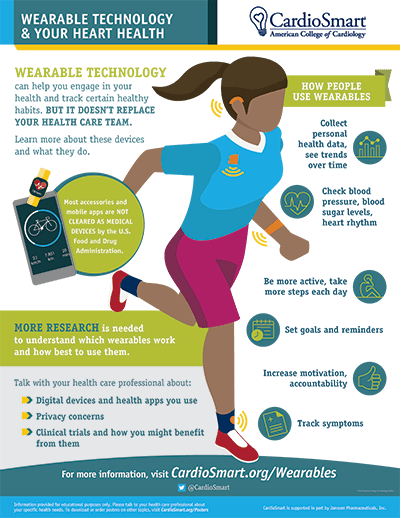
They discuss updates in the diagnosis and management of heart failure, including wearables, biomarkers, the 4 pillars of therapy, and how and why there has historically been an under-representation of women in heart failure trials. This episode is sponsored by an educational grant from the Boehringer Ingelheim-Lilly Alliance. The sponsor has no influence over podcast content, the selection of speakers or any associated educational material.
Professor Carolyn Lam is a Senior Consultant from the Department of Cardiology and Director of Women’s Heart Health at the National Heart Centre Singapore, having pioneered the first Women’s Heart Clinic in Singapore. Academically, she serves as a tenured Full Professor at the Duke-National University of Singapore, having also graduated from the Standford Executive Programme in 2015, and obtained a PhD at the University Medical Centre Groningen, the Netherlands in 2016. In the field of MedTech, Prof Lam is co-founder of Us2.ai, an award-wining startup dedicated to the automation of the fight against heart disease by applying artificial intelligence to echocardiography (ultrasound of the heart).
Prof Lam is a world-renowned specialist in heart failure (particularly heart failure with preserved ejection fraction [HFpEF]). Her work in the PARAGON-HF and EMPEROR-Preserved trials led to the first FDA-approved treatment for HFpEF and the first robustly positive clinical outcomes trial in HFpEF to-date, respectively. She leads several multinational global and regional clinical trials, and has received numerous prestigious awards and global recognition for her work. Her recent appointments on the 2021 European Society of Cardiology Heart Failure Guidelines Task Force, and as International Honorary Fellow of the Heart Failure Society of America 2021, attest to her contributions in both cardiology and research fields.
Prof Lam is a proud recipient of the National Medical Research Council (NMRC) Senior Investigator Clinician Scientist Award in 2020, and served as the Founding Programme Lead of A*STaR’s Asian neTwork for Translational Research and Cardiovascular Trials (ATTRaCT) and Principal Investigator of ASIAN-HF (a multinational study across 11 Asian countries). In 2019, She initiated the Asian Diabetes Outcomes Prevention Trial (ADOPT), an ongoing trial involving 5 countries and aimed at reducing the cardiovascular adverse outcomes of diabetes in Asian patients.
She has published with over 350 articles in major high impact journals including New England Journal of Medicine, Journal of the American Medical Association (JAMA), Lancet, Circulation, and European Heart Journal; and has been recognised as a World Expert by Expertscape’s PubMed-based algorithms (top 0.1% of scholars writing about Heart Failure over the past 10 years; Heart Failure: Worldwide – Expertscape.com). Besides being an Associate Editor for Circulation (top Cardiology Journal) and European Journal of Heart Failure, she is also the lead author of the chapter on HFpEF for Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine, 12th Edition – the award-winning textbook trusted by generations of cardiologists for the latest, most reliable guidance in the field.