DR. C REVIEWS MAJOR MEDICAL NEWS FOR THE WEEK ENDING JUNE 20, 2020.
Tag Archives: Coronavirus
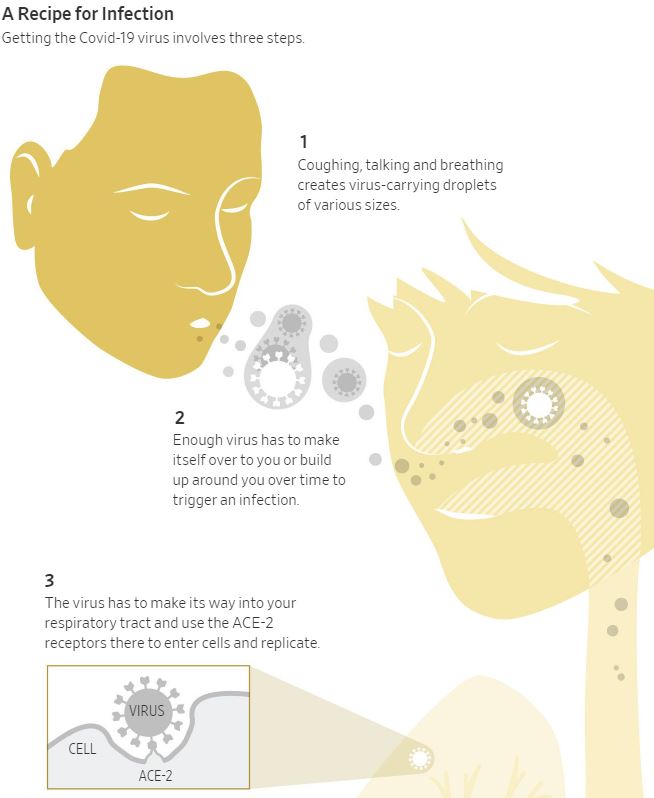
CORONAVIRUS: RESPIRATORY-DROPLET CONTACT IS MAJOR WAY COVID-19 SPREADS
From the Wall Street Journal (June 16, 2020):
Health agencies have so far identified respiratory-droplet contact as the major mode of Covid-19 transmission. These large fluid droplets can transfer virus from one person to another if they land on the eyes, nose or mouth. But they tend to fall to the ground or on other surfaces pretty quickly.
Some researchers say the new coronavirus can also be transmitted through aerosols, or minuscule droplets that float in the air longer than large droplets. These aerosols can be directly inhaled.
Sufficient ventilation in the places people visit and work is very important, said Yuguo Li, one of the authors and an engineering professor at the University of Hong Kong. Proper ventilation—such as forcing air toward the ceiling and pumping it outside, or bringing fresh air into a room—dilutes the amount of virus in a space, lowering the risk of infection.
Another factor is prolonged exposure. That’s generally defined as 15 minutes or more of unprotected contact with someone less than 6 feet away, said John Brooks, the Centers for Disease Control and Prevention’s chief medical officer for the Covid-19 response. But that is only a rule of thumb, he cautioned. It could take much less time with a sneeze in the face or other intimate contact where a lot of respiratory droplets are emitted, he said.
INFOGRAPHICS: “COVID-19 COMPARED TO OTHER DISEASES AND CONDITIONS”

PODCAST INTERVIEWS: DIAGNOSIS AND EARLY TREATMENT OF COVID-19
In this audio interview conducted on June 3, 2020, the editors discuss two new studies: one comparing test swabs collected by health care workers with swabs collected by the patients themselves and one assessing hydroxychloroquine treatment in people who had been exposed to Covid-19 but weren’t yet ill.
The continuing spread of SARS-CoV-2 remains a Public Health Emergency of International Concern. What physicians need to know about transmission, diagnosis, and treatment of Covid-19 is the subject of ongoing updates from infectious disease experts at the Journal.
Eric Rubin is the Editor-in-Chief of the Journal. Lindsey Baden is a Deputy Editor of the Journal. Stephen Morrissey, the interviewer, is the Executive Managing Editor of the Journal.
HEALTH: HOW SLEEP HAS CHANGED DURING COVID-19
From the Wall Street Journal (June 1, 2020):
“The biggest problem has been staying asleep,” says Philip Muskin, a professor of psychiatry at Columbia University Medical Center in New York. “People aren’t exercising, their days have no structure at all.”

Preliminary results from a survey taken by around 1,600 people from 60 countries show that 46% reported poor sleep during the pandemic, while only 25% said they had slept poorly before it, according to Melinda Jackson, a senior lecturer at the Turner Institute for Brain and Mental Health at Monash University in Melbourne, who studies how stressful events affect people’s sleep. Forty percent also reported increased alcohol consumption.
The key is to prevent the sleep problem from becoming chronic, she says. It is important to avoid associating your bed or bedroom with a place where you are awake. Experts recommend that if you can’t fall asleep, or wake up in the middle of the night and are unable to go back to sleep after 20 minutes, get out of bed and do something relaxing.
COVID-19: CASE SEVERITY IS DEPENDENT ON VIRAL LOAD
From the New York Times
….in the case of the new coronavirus, people who have no symptoms seem to have viral loads — that is, the amount of virus in their bodies — just as high as those who are seriously ill, according to some studies.

When experts recommend wearing masks, staying at least six feet away from others, washing your hands frequently and avoiding crowded spaces, what they’re really saying is: Try to minimize the amount of virus you encounter.
A few viral particles cannot make you sick — the immune system would vanquish the intruders before they could. But how much virus is needed for an infection to take root? What is the minimum effective dose?
And coronavirus patients are most infectious two to three days before symptoms begin, less so after the illness really hits.
Some people are generous transmitters of the coronavirus; others are stingy. So-called super-spreaders seem to be particularly gifted in transmitting it, although it’s unclear whether that’s because of their biology or their behavior.
On the receiving end, the shape of a person’s nostrils and the amount of nose hair and mucus present — as well as the distribution of certain cellular receptors in the airway that the virus needs to latch on to — can all influence how much virus it takes to become infected.
COMMENTARY
HEALTH: THE HISTORY OF FACEMASKS AND DISEASE THROUGH THE CENTURIES
Originating during the Black Death of the Middle Ages, face coverings to protect against the transmission of disease are not just medical requirements; they’re now a fashion statement. Mark Phillips talks with medical historian Mark Honigsbaum (“The Pandemic Century”) about the purpose and style of facemasks.
COMMENTARY
Medicine has always operated in the context of theory, which is easier to generate than fact. The medieval physician with the “bird mask” thought he was protecting himself from “miasma”, which was theorized to be the means by which PLAGUE was spread. In fact, the masks’ main function was to hide his identity from his Patient, whom he could not help. The painting makes him appear to be the Grim Reaper himself.
The story of Guaiac, another illustration medieval medicine, is entwined with Syphillis, the stigmatizing STD of post Columbian Europe. Each country blamed Syphillis on its’ rival- the English called it the French disease, for instance-until they were able to blame it on the “new world”. Since it came from the Americas, so must its’ HERBAL REMEDY, according to theory.
GUAIAIC, the resin from the small tree from the Caribbean, became a popular cure. It might have even lessened suffering from Siphillis, since it was used instead of the highly toxic MERCURY.
Guaiac eventually found a use in Criminology, as a test for blood at the crime scene. When Guaiac is mixed with a suspicious spot and peroxide, it changes color rapidly to a bright blue. Medicine later used Guaiac as a test for hidden (occult) Blood In the stool; a positive, brilliant blue test throws suspicion on intestinal cancer as the culprit.
We come full circle to present day mask usage in the Covid epidemic. Some countries outlaw masks because masks interfere with criminal investigation. This interdict had to be relaxed during The Pandemic. How convenient for the rioters and looters in Minnesota!
—Dr. C.
CORONAVIRUS: CONFUSING HYDROXYCHLOROQUINE STUDIES (NATURE PODCAST)
President Trump’s preferred coronavirus treatment is the focus of a new study suggesting it could cause more harm than good, but not everybody agrees. We discuss the fallout as trials around the world are paused and countries diverge over policy advice.
12:12 Are we rushing science?
Coronavirus papers are being published extremely quickly, while normally healthy scientific debate is being blown up in the world’s press. Is there a balancing act between timely research and accurate messaging?
18:49 One good thing
Our hosts pick out things that have made them smile in the last week, including hedgerow brews and a trip into the past using AI.
Recipe: Elderflower ‘Champagne’
Video: Denis Shiryaev restores historic footage with AI
22:30 The latest coronavirus research papers
Noah Baker takes a look through some of the key coronavirus papers of the last few weeks.
News: Coronavirus research updates
medRxiv: Full genome viral sequences inform patterns of SARS-CoV-2 spread into and within Israel
Harvard Library: Reductions in commuting mobility predict geographic differences in SARS-CoV-2 prevalence in New York City
Science: DNA vaccine protection against SARS-CoV-2 in rhesus macaques
VIDEO: “IS TELEMEDICINE THE FUTURE OF HEALTH CARE?”
The coronavirus pandemic has overwhelmed hospitals, physicians and the medical community. That’s pushed telemedicine into the hands of providers and patients as the first response for primary care. Telemedicine isn’t new to the medical community, however it hasn’t been embraced due to insurance coverage, mindset and stigma. Here’s how it works and what it means for the future of health care.
COMMENTARY
The safety and convenience of Telemedicine have been amply illustrated by Covid 19. It’s place in the future of Medicine would seem to be assured.
Once the epidemic is over, however, some sticky details, waved away by fiat during the early days, must be addressed.
Will Payment parity be allowed by the Health insurance companies (And Medicare) be continued? Will cross-border Practice still be allowed by the states. Will more Doctors modernize? Will lawyers (and litigious patients) restrain themselves?
Stay Tuned!
—Dr. C.
HEALTH: “HOW THE BODY CLEARS COVID-19” (VIDEO)
Understanding how the body clears the new coronavirus is becoming more important as the U.S. begins to reopen. WSJ’s Daniela Hernandez explains how the body fights infection and why feeling better doesn’t equal being virus-free. Photo illustration: Laura Kammermann
COMMENTARY
This excellent video is well worth watching and listening to. It revisits how the immune system, both innate and adaptive responds to SARS CoV and other viruses.
It shows graphically how long the body takes to clear the the Covid 19 virus.

And it makes me, a susceptible 88 year old, even more alert to infection. We should keep our guards up.
Even if an effective vaccine is found, it will probably take its place, incorporated into influenza vaccine as an annual immunization.









