If you’re enrolled only in original Medicare with a Medigap supplemental plan, and don’t use a drug plan, there’s no need to re-evaluate your coverage, experts say. But Part D drug plans should be reviewed annually. The same applies to Advantage plans, which often wrap in prescription coverage and can make changes to their rosters of in-network health care providers.

“The amount of information that consumers need to grasp is dizzying, and it turns them off from doing a search,” Mr. Riccardi said. “They feel paralyzed about making a choice, and some just don’t think there is a more affordable plan out there for them.”
Is there another way?

When creation of the prescription drug benefit was being debated, progressive Medicare advocates fought to expand the existing program to include drug coverage, funded by a standard premium, similar to the structure of Part B. The standard Part B premium this year is $144.60; the only exceptions to that are high-income enrollees, who pay special income-related surcharges, and very low-income enrollees, who are eligible for special subsidies to help them meet Medicare costs.
“Given the enormous Medicare population that could be negotiated for, I think most drugs could be offered through a standard Medicare plan,” said Judith A. Stein, executive director of the Center for Medicare Advocacy.
“Instead, we have this very fragmented system that assumes very savvy, active consumers will somehow shop among dozens of plan options to see what drugs are available and at what cost with all the myriad co-pays and cost-sharing options,” she added.
Advocates like Ms. Stein also urged controlling program costs by allowing Medicare to negotiate drug prices with pharmaceutical companies — something the legislation that created Part D forbids.
COMMENTARY
Medicare is a blessing. It is a great help to retired and elderly people and generally does the job it was intended to do. There are a great variety of Medicare supplement plans and pharmaceutical purchase plans, And they jockey and change every year.
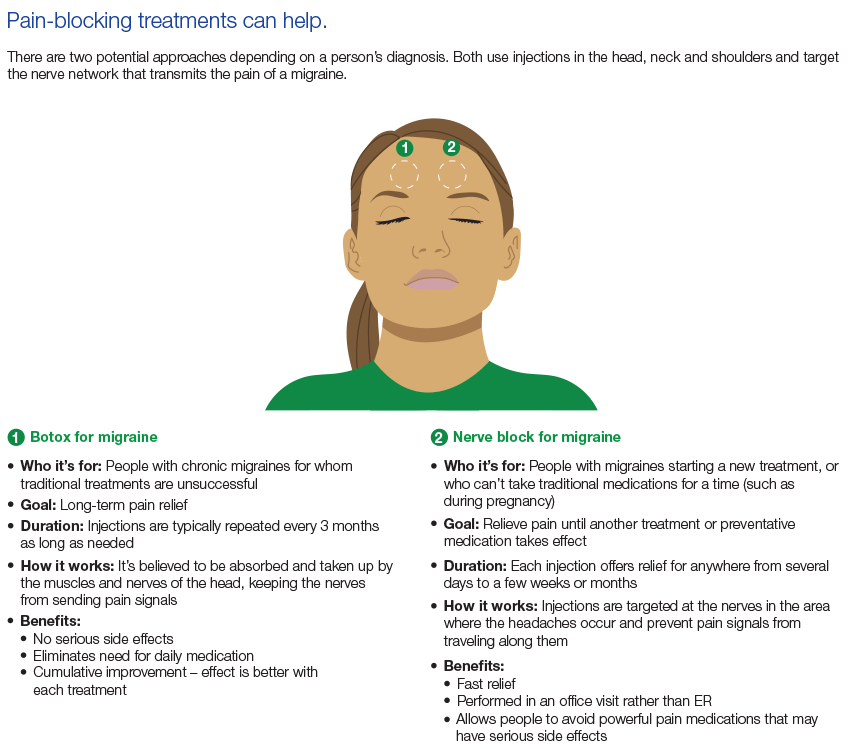
I get a headache just thinking about how to compare these plans from my individual needs and and whether their cost is worth it. The take-home message from the New York Times article is that you can get individual attention from an advisor who presumably knows the field well.
The key acronyms are SHIP and HICAP, which stands for state health insurance assist program and California health insurance counseling and advisor program respectively.
The California number is 1-800-434-0222. Be sure to write down the medications that you are taking and Your diagnosed illnesses, as well as your financial status in order to make best use of the service.
—Dr. C.