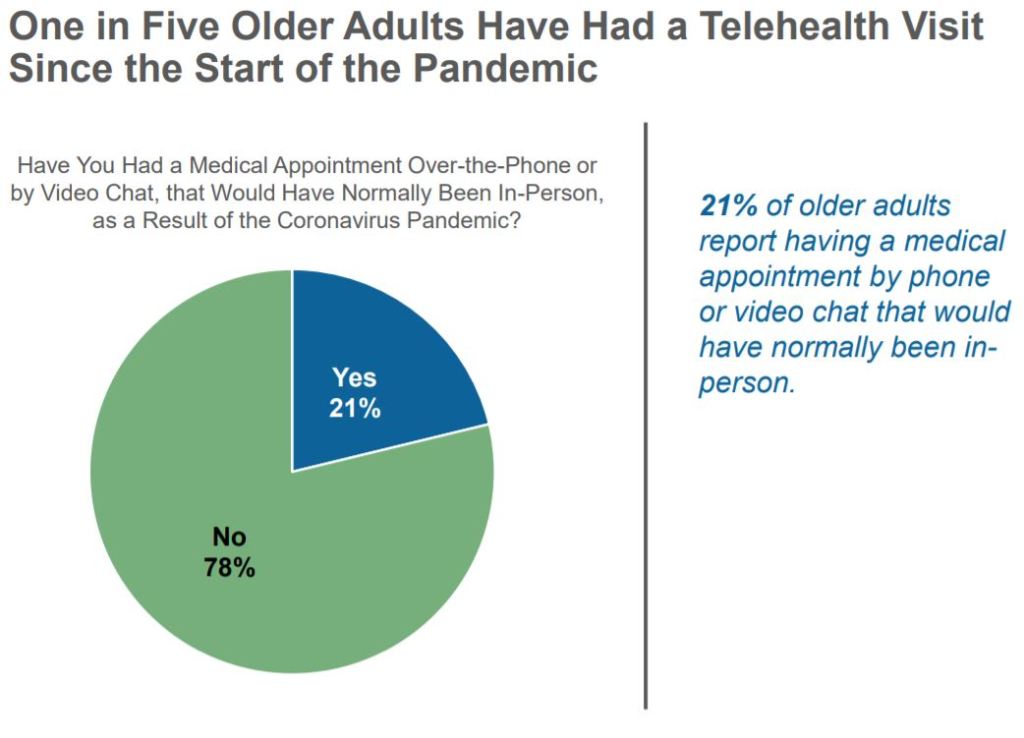
Amid the Covid-19 pandemic, more doctors are turning to telemedicine. That’s a problem for tens of millions on the wrong side of the digital divide.
SPEAKING ON A landline, the patient complained of an itchy eye. On the call’s other end, physician Carla Harwell considered the possibilities, from seasonal allergies to vision-damaging herpes. Luckily, the elderly patient’s daughter was visiting during the phone consultation, so Harwell asked her to text a picture of her mom’s eye. The photo shocked Harwell. It was the worst case of bacterial conjunctivitis the doctor had ever seen.

Without the picture, Harwell would have told the octogenarian patient to call back in a few days or come to her office, risking an in-patient visit during the Covid-19 pandemic. She certainly wouldn’t have prescribed the antibacterial eye drops needed to treat the infection. “I probably would not have prescribed anything,” Harwell says. “That’s a scary thought.”
COMMENTARY
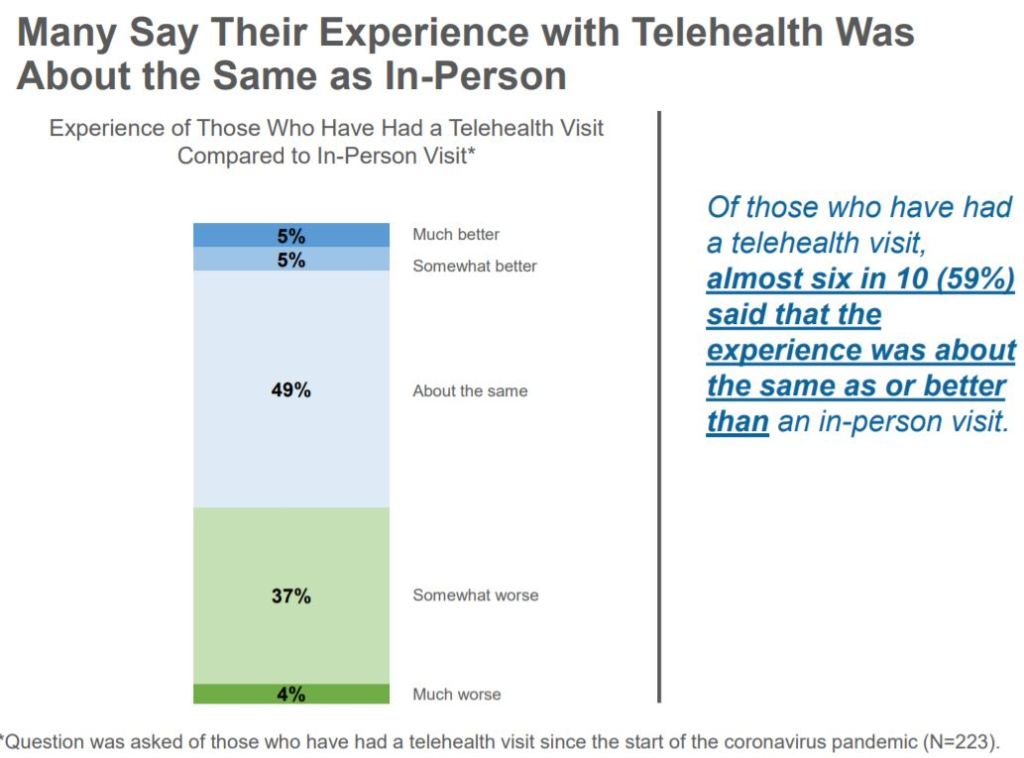
Telehealth is here, will remain after the pandemic, and is useful in many situations.
Being older, poorer, minority, Linguistically challenged, rural, less informed and less Tech-savvy reinforce each other in comprising Barriers to proper Medical care of ANY kind, especially Telemedicine. These handicaps will hopefully improve with time, and should be A societal priority.
Special internet-connected roving Aid-mobiles in afflicted areas is one feasible idea that would help. Responding to a lesser “911” number, the health-van could go to the calling persons location, help the person to the van, take pictures and other data for a Telehealth Doctor to evaluate, and facilitate treatment.
A neighborhood Telehealth site is also workable, and was a precondition to Rural Telehealth access, pre-pandemic.
If you are reading this message, congratulations! You are increasing your information, technical facility and your access to better Healthcare.