Our bodies have evolved in a binary environment that cycles between day and night, which impose different demands for the optimal functioning of our bodies.
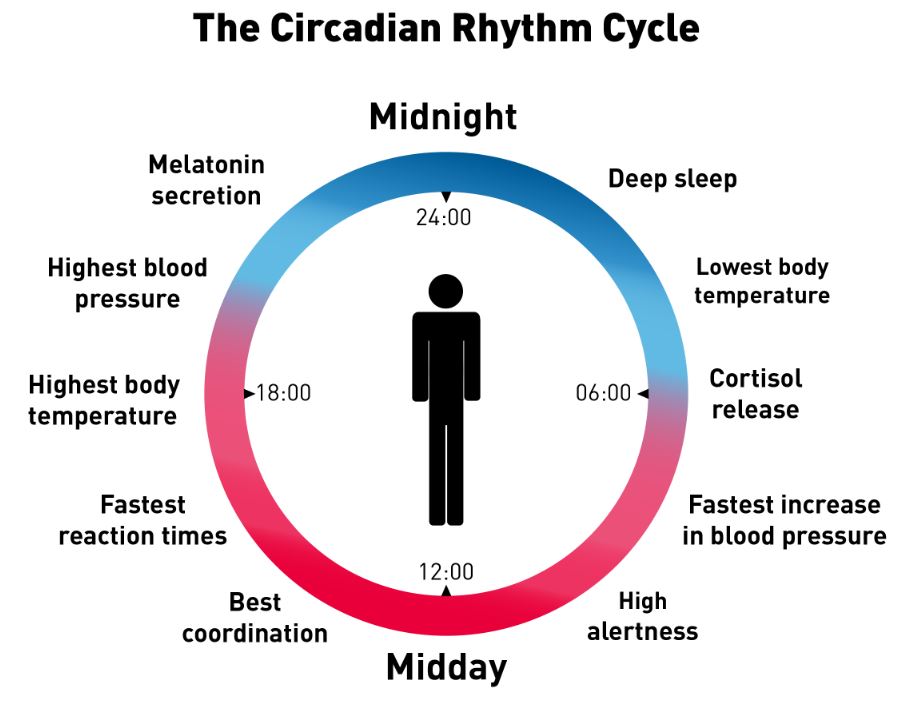
In the daytime, we typically explore, fight and eat. In the night time we rest and digest.
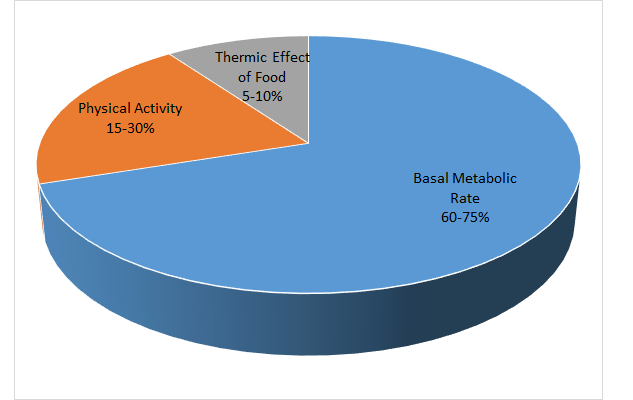
We have an unconscious, or autonomic, nervous system, that helps us adjust, the sympathetic nervous system revving us up for the daytime, and the parasympathetic, including the vagus nerve, slowing us down at night time. Sleep has apparently evolved to repair, cleanse and grow our bodies at night, in a process called anabolism. In the daytime, we have wear and tear, and use more energy to survive in a metabolic process called catabolism.
Hormones and Neurotransmitters help time and facilitate these cycling processes.
Light In the morning, operating through the central “zeitgeber” in the supachiasmatic nucleus, synchronizes the circadian rhythm present in each of our cells, and drives down melatonin. Cortisol rises to help with stress, adenosine rises because of muscular and neural activity, the sympathetic nervous system is more active to help with alertness and raise the blood pressure, pulse rate, and body temperature.
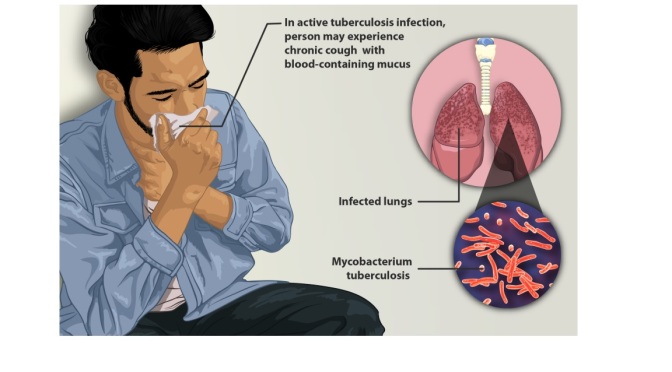
As the light decreases at night, the melatonin Increases to facilitate sleep. Cortisol decreases, allowing the immune system to become more active, with immune lymphocytes going into the lymph nodes to start dealing with any infection that has been encountered during the day. The daytime diet is being digested, replenishing the ATP and glycogen energy stores in muscle, brain and other tissues. Growth hormone signals cells to divide, and helps children grow.
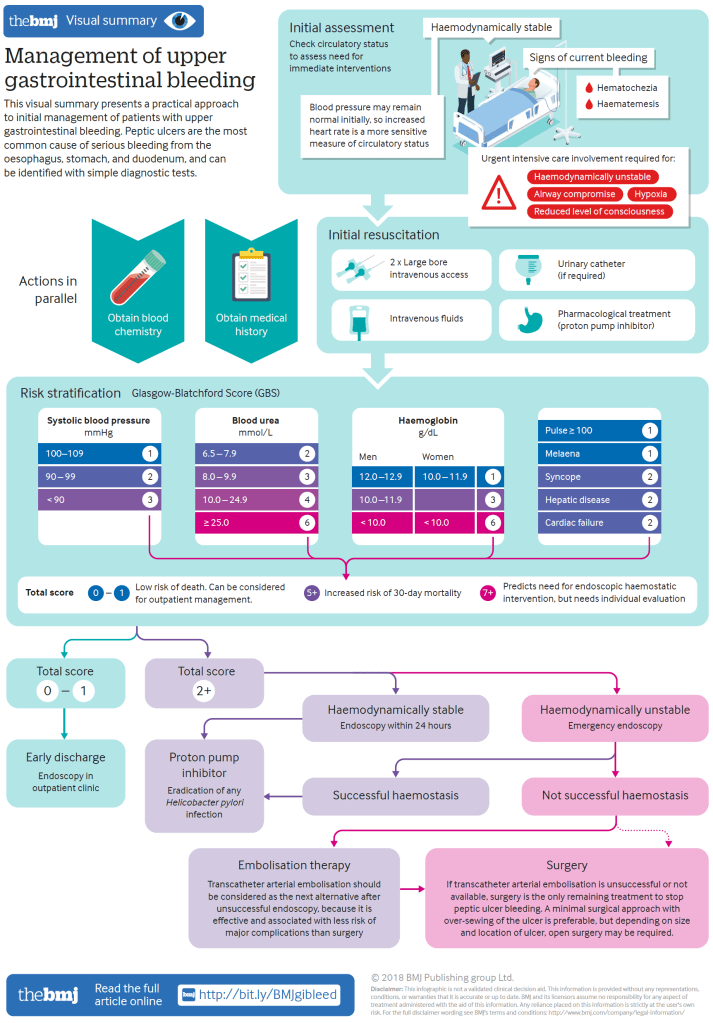
Medical science makes use of this information in a field called chronotherapy. Cancer treatment with radiation and radiomimetic drugs are best done at night, when the cells divide. Asthma medications are often given at night, because asthma is more common with a decrease in cortisol. GERD medications, such as proton pump inhibitors, are best given at night, because gastric acid builds up then, and lying flat encourages any acidic food to reflux into the esophagus.
As I have always mentioned, sleep, diet, and exercise are important for best health.
A sleep hygiene routine, going to bed by 10 PM and getting 7 to 8 hours of sleep is critical to give the body time to repair itself. Getting enough exercise will increase adenosine and facilitate a good nights sleep, along with countless other beneficial effects. Avoiding blue light from television and computer screens in the evening will help melatonin increase for good nights sleep. Avoiding food for three or four hours before bedtime will allow time to get the food out of the stomach and reduce gastroesophageal reflux.
TRE, or time restricted eating, is a form of fasting, which correlates with longevity.
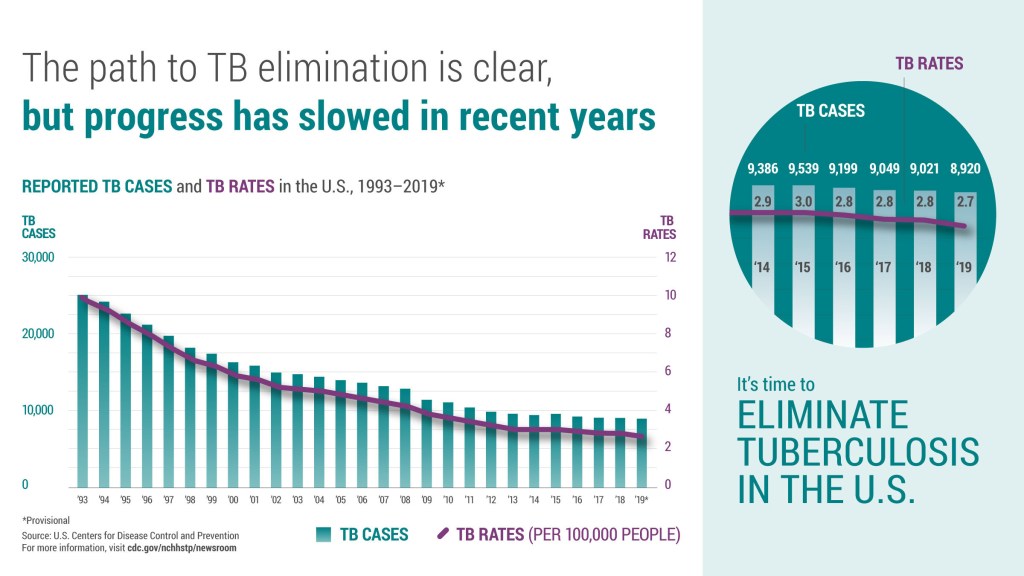
Help the body synchronize its circadian clocks by well-timed, regular habits, and you will have a far better chance to be healthy. You are on dangerous grounds if you foul up the circadian rhythm by staying awake until the wee hours, eating an unhealthy diet and snacking all the time on lots of carbohydrates with little fiber, and sit around without exercising. Obesity, metabolic syndrome, diabetes, and gastrointestinal illnesses, as well as cancer can result.
Night shift work, for example, disturbs our biological clock, and has recently been labeled as carcinogenic.
—Dr. C.