Artificial intelligence reduced by twofold the rate at which precancerous polyps were missed in colorectal cancer screening, reported a team of international researchers led by Mayo Clinic. The study is published in Gastroenterology.
Tag Archives: Medicine
Infographic: Diagnosis Of Gastrointestinal Pain
Neurovascular Disease: Stroke Awareness & Care
Mayo Clinic’s Eugene L. Scharf, M.D., Robert D. Brown Jr., M.D., M.P.H. and Harry Cloft, M.D., Ph.D. discuss how the team at Mayo Clinic provides each patient individualized care to help maximize quality of life. 700,000 to 800,000 people in the United States have a stroke each year. Many people can lower their risk of stroke with medical risk factor modification. When a stroke occurs, prompt treatment is crucial. Every minute counts and can reduce brain damage and other complications. “Some patients who would have had a devastating stroke come out of the hospital with no deficient, no difficulties whatsoever,” says Robert D. Brown Jr., M.D., M.P.H.
Chronic Conditions: Non-Union Bone Fractures
DOCTORS PODCAST: MEDICAL & TELEHEALTH NEWS (APR 3)
A weekly podcast on the latest medical, science and telehealth news.
Back Pain: The Causes & Symptoms Of Sciatica
Sciatica refers to pain caused by the sciatic nerve that carries messages from the brain down the spinal cord to the legs. The pain of sciatica typically radiates down one side from the lower back into the leg, often below the knee. The most common cause is a bulging (“herniated”) disc in the lower back. Discs are tire-like structures that sit between the bones of the spine. If the outer rim of the disc tears, usually due to routine pressure on the lower back, the jelly-like inner material can come out and pinch or inflame the nearby nerve. Sciatica is most common in people 30 to 50.
How do you know if it is sciatica?
The key to diagnosing sciatica is a thorough history and a focused exam. Sciatica symptoms are often worse with sitting or coughing and may be accompanied by numbness or tingling in the leg. A physical exam can confirm that the sciatic nerve is involved. If there is muscle weakness or diminished reflexes in the involved leg, an imaging test such as a back MRI can be useful and help guide a decision for early surgery.
Intestines: Leaky Gut – Symptoms & Diagnosis
Inside our bellies, we have an extensive intestinal lining covering more than 4,000 square feet of surface area. When working properly, it forms a tight barrier that controls what gets absorbed into the bloodstream. An unhealthy gut lining may have large cracks or holes, allowing partially digested food, toxins, and bugs to penetrate the tissues beneath it. This may trigger inflammation and changes in the gut flora (normal bacteria) that could lead to problems within the digestive tract and beyond. The research world is booming today with studies showing that modifications in the intestinal bacteria and inflammation may play a role in the development of several common chronic diseases.
Cancer Diagnosis: The Symptoms Of Lymphoma
Knowing the symptoms of Lymphoma is essential for diagnosis and early treatment. Painless lumps near the lymph nodes, extreme fatigue, high fever and significant weight loss without a known cause are all signs to watch for.
Chapters: 0:00 Intro 0:15 Lymphoma overview 0:46 3 “b-symptoms” of lymphoma 1:09 Other warning signs of lymphoma 2:11 When to contact your healthcare provider
The IGA Immune System And Nasal Immunization
The IGA immune system comprises approximately 2/3 of all the immune cells in the body. Intestinal tract, respiratory tract, and skin are all exterior surfaces and are required to hold the environments’ many pathogens at bay.
IGA is one of several classes of immunoglobulins, the others being Gamma M, Gamma E, and several sub classes of Gamma G. They each have different structures and functions, but all have the basic underlying mechanisms of antigen presentation, clonal expansion, heavy chain and light chain dimers and specificity.
Mucosal gamma A occurs in pairs, with a junctional J chain and a secretory piece; The latter serves as a type of receptor on the cell surface; Imagine millions of gamma A combining sites waving on the surface of respiratory and intestinal epithelium waiting for pathogens to come along. Once combined with the virus or bacterium, they are shed into the mucus and eliminated before the virus can get to the mucosal cells.
With an IM injection of COVID-19 vaccine, all of the immunoglobulin classes except for Gamma E respond, with the earliest anybody at four or five days and peaking at 11 to 12 days. Gamma A in the serum occurs as a single antibody, as opposed to the secretory IGA which occur in pairs. Gamma G and M reside in the serum, and do not occur in any significant amounts in the mucus, leaving secretory gamma A alone to directly face the outside world.
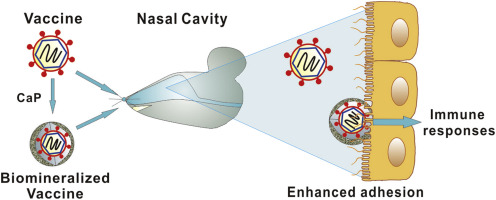
Nasal immunization should theoretically be the route of choice for respiratory viruses. There is a vigorous response not only in the production of mucosal secretory IGA, but also in the production of serum immunoglobulins including IgG. However, the Titanic of medical practice turns very slowly. Part of the problem is probably tradition; immunizations have always been given by subcutaneous or intramuscular injection.
When a substance is injected, you know that it’s in the body in a precise amount, the tissues are very vascular, and the pick up rate is known, and it works well. With IM immunizations, people may get sick, because the lining membranes are not protected, but the immunized person rapidly produces huge amounts of IgG which usually keeps the infection under control. Covid is unique in its ability to evade the innate immune system, and multiply rapidly before the humoral immune response is adequate. Also, Covid Immunity wanes rapidly, aided by the fact that Covid is always changing it’s outer form.
There are more than a dozen nasal Covid vaccines being investigated, and the early studies on hamsters and mice showed a robust mucosal antibody production as well as a serum IgG production at least as great as intramuscular injection.
There are, however, several problems. An attenuated, live COVID-19 vaccine would theoretically be the best, since the virus itself is able to get into the cells and start replicating. However, lack of experience makes the medical profession fearful. There are a huge number of “do not give to” warnings on the only currently approved nasal vaccine, which is an attenuated influenza virus. There are worries about immunodeficient people, older people, pregnant people and about the possibility that the attenuated virus will go into the central nervous system via the olfactory system.
There are practical concerns as well. Viral vector vaccines may stimulate an amnestic response to the vector that excludes the vaccine from entering the cells. The nasal vaccine might be swept away with the mucus. How much is the vaccine will remain in the nasal tissues? Will patients have any confidence in the vaccine since it’s just a spray in the nose? Will it be abused, since literally anybody could administer the nasal vaccine.
The bottom line is that of the many vaccines in trial, not a single one is expected to be approved until the early fall. Interestingly, Pfizer is working with an mRNA nasal vaccine. DNA nasal vaccines are also being tried, since DNA is a more stable molecule. A number of adenoviral vectored vaccines are in trials.
The nasal route for immunization is so promising that I believe we will eventually have nasal vaccines, hopefully tailored for current viral variants.
Nasal antibody administration, or a small molecule drug that will combine with Covid are being looked at, but since they do not produce more than transient effects, I doubt if they will be very popular. Carrageenan is an approved substance that ties up viruses, and might have a chance to succeed as a nasal spray treatment.
Pills are so much for more familiar to people as a treatment device, and seem more attractive to drug companies. I do not believe that nasal sprays will replace them as the staple of outpatient medical treatment.
—Dr. C.
Inflammation: Three Ways It Affects Your Health
Acute inflammation happens as a part of our defense mechanism to clear out pathogens. So when a virus or bacteria invades us, we need to quickly mount an acute inflammatory response to get rid of the pathogen. Sometimes, that acute immune response isn’t enough to get rid of the pathogen. That’s when we elevate the level to the adaptive immune response. That’s when you involve specific lymphocytes, T and B cells, to fight off the infection.
So inflammation is a necessary process for dealing with pathogens but sometimes, it can also turn against us. Chronic inflammation happens because the body fails to get rid of the cause of the inflammation, such as viruses and bacteria. In those conditions, such as, you know, chronic infection with HIV or hepatitis virus or lung COVID, in which case we there may be a persistent viral reservoir that’s causing this chronic inflammation, the inflammation itself becomes the enemy.
Even though inflammation evolve to counter pathogens, it’s also engaged by other causes, and so having this amount of fat, for example, alone is able to trigger the immune system and induce the chronic inflammatory response that then fuels further problems to happen because the body is sort of trying to fight off a non-existent infection and therefore, it can sort of engage a chronic state of inflammation.
I can’t think of a disease which doesn’t involve inflammation, but we are now learning more and more about the physiological role of inflammation. Homeostasis ensures that we have a normal operation of different physiological functions like heart rate, breathing and glucose levels or insulin levels. Those two system, the inflammatory system and the homeostasis, they work together to maintain each other. Sometimes, the inflammatory response has to override the homeostatic response.
That includes things like adaptation to a different diet. The immune cells are now known to be able to sense differences in dietary conditions and adapt the intestine for future absorption of nutrients. This kind of events that are not necessarily at all related to pathogens, but for maintaining physiology. Inflammatory responses are integral in order to maintain health. So a molecular-level understanding of inflammation is necessary to understand the logic by which these systems function, and also it provides the pharmaceutical target for future therapies of inflammatory diseases.










