Inside our bellies, we have an extensive intestinal lining covering more than 4,000 square feet of surface area. When working properly, it forms a tight barrier that controls what gets absorbed into the bloodstream. An unhealthy gut lining may have large cracks or holes, allowing partially digested food, toxins, and bugs to penetrate the tissues beneath it. This may trigger inflammation and changes in the gut flora (normal bacteria) that could lead to problems within the digestive tract and beyond. The research world is booming today with studies showing that modifications in the intestinal bacteria and inflammation may play a role in the development of several common chronic diseases.
Cancer Diagnosis: The Symptoms Of Lymphoma
Knowing the symptoms of Lymphoma is essential for diagnosis and early treatment. Painless lumps near the lymph nodes, extreme fatigue, high fever and significant weight loss without a known cause are all signs to watch for.
Chapters: 0:00 Intro 0:15 Lymphoma overview 0:46 3 “b-symptoms” of lymphoma 1:09 Other warning signs of lymphoma 2:11 When to contact your healthcare provider
The IGA Immune System And Nasal Immunization
The IGA immune system comprises approximately 2/3 of all the immune cells in the body. Intestinal tract, respiratory tract, and skin are all exterior surfaces and are required to hold the environments’ many pathogens at bay.
IGA is one of several classes of immunoglobulins, the others being Gamma M, Gamma E, and several sub classes of Gamma G. They each have different structures and functions, but all have the basic underlying mechanisms of antigen presentation, clonal expansion, heavy chain and light chain dimers and specificity.
Mucosal gamma A occurs in pairs, with a junctional J chain and a secretory piece; The latter serves as a type of receptor on the cell surface; Imagine millions of gamma A combining sites waving on the surface of respiratory and intestinal epithelium waiting for pathogens to come along. Once combined with the virus or bacterium, they are shed into the mucus and eliminated before the virus can get to the mucosal cells.
With an IM injection of COVID-19 vaccine, all of the immunoglobulin classes except for Gamma E respond, with the earliest anybody at four or five days and peaking at 11 to 12 days. Gamma A in the serum occurs as a single antibody, as opposed to the secretory IGA which occur in pairs. Gamma G and M reside in the serum, and do not occur in any significant amounts in the mucus, leaving secretory gamma A alone to directly face the outside world.
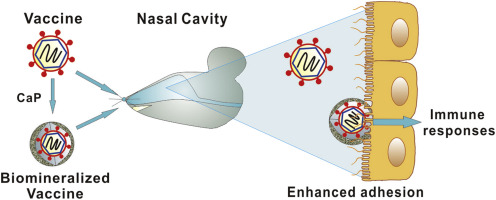
Nasal immunization should theoretically be the route of choice for respiratory viruses. There is a vigorous response not only in the production of mucosal secretory IGA, but also in the production of serum immunoglobulins including IgG. However, the Titanic of medical practice turns very slowly. Part of the problem is probably tradition; immunizations have always been given by subcutaneous or intramuscular injection.
When a substance is injected, you know that it’s in the body in a precise amount, the tissues are very vascular, and the pick up rate is known, and it works well. With IM immunizations, people may get sick, because the lining membranes are not protected, but the immunized person rapidly produces huge amounts of IgG which usually keeps the infection under control. Covid is unique in its ability to evade the innate immune system, and multiply rapidly before the humoral immune response is adequate. Also, Covid Immunity wanes rapidly, aided by the fact that Covid is always changing it’s outer form.
There are more than a dozen nasal Covid vaccines being investigated, and the early studies on hamsters and mice showed a robust mucosal antibody production as well as a serum IgG production at least as great as intramuscular injection.
There are, however, several problems. An attenuated, live COVID-19 vaccine would theoretically be the best, since the virus itself is able to get into the cells and start replicating. However, lack of experience makes the medical profession fearful. There are a huge number of “do not give to” warnings on the only currently approved nasal vaccine, which is an attenuated influenza virus. There are worries about immunodeficient people, older people, pregnant people and about the possibility that the attenuated virus will go into the central nervous system via the olfactory system.
There are practical concerns as well. Viral vector vaccines may stimulate an amnestic response to the vector that excludes the vaccine from entering the cells. The nasal vaccine might be swept away with the mucus. How much is the vaccine will remain in the nasal tissues? Will patients have any confidence in the vaccine since it’s just a spray in the nose? Will it be abused, since literally anybody could administer the nasal vaccine.
The bottom line is that of the many vaccines in trial, not a single one is expected to be approved until the early fall. Interestingly, Pfizer is working with an mRNA nasal vaccine. DNA nasal vaccines are also being tried, since DNA is a more stable molecule. A number of adenoviral vectored vaccines are in trials.
The nasal route for immunization is so promising that I believe we will eventually have nasal vaccines, hopefully tailored for current viral variants.
Nasal antibody administration, or a small molecule drug that will combine with Covid are being looked at, but since they do not produce more than transient effects, I doubt if they will be very popular. Carrageenan is an approved substance that ties up viruses, and might have a chance to succeed as a nasal spray treatment.
Pills are so much for more familiar to people as a treatment device, and seem more attractive to drug companies. I do not believe that nasal sprays will replace them as the staple of outpatient medical treatment.
—Dr. C.
Inflammation: Three Ways It Affects Your Health
Acute inflammation happens as a part of our defense mechanism to clear out pathogens. So when a virus or bacteria invades us, we need to quickly mount an acute inflammatory response to get rid of the pathogen. Sometimes, that acute immune response isn’t enough to get rid of the pathogen. That’s when we elevate the level to the adaptive immune response. That’s when you involve specific lymphocytes, T and B cells, to fight off the infection.
So inflammation is a necessary process for dealing with pathogens but sometimes, it can also turn against us. Chronic inflammation happens because the body fails to get rid of the cause of the inflammation, such as viruses and bacteria. In those conditions, such as, you know, chronic infection with HIV or hepatitis virus or lung COVID, in which case we there may be a persistent viral reservoir that’s causing this chronic inflammation, the inflammation itself becomes the enemy.
Even though inflammation evolve to counter pathogens, it’s also engaged by other causes, and so having this amount of fat, for example, alone is able to trigger the immune system and induce the chronic inflammatory response that then fuels further problems to happen because the body is sort of trying to fight off a non-existent infection and therefore, it can sort of engage a chronic state of inflammation.
I can’t think of a disease which doesn’t involve inflammation, but we are now learning more and more about the physiological role of inflammation. Homeostasis ensures that we have a normal operation of different physiological functions like heart rate, breathing and glucose levels or insulin levels. Those two system, the inflammatory system and the homeostasis, they work together to maintain each other. Sometimes, the inflammatory response has to override the homeostatic response.
That includes things like adaptation to a different diet. The immune cells are now known to be able to sense differences in dietary conditions and adapt the intestine for future absorption of nutrients. This kind of events that are not necessarily at all related to pathogens, but for maintaining physiology. Inflammatory responses are integral in order to maintain health. So a molecular-level understanding of inflammation is necessary to understand the logic by which these systems function, and also it provides the pharmaceutical target for future therapies of inflammatory diseases.
Diet & Nutrition: Nine Healthy ‘Brain Food’ Tips
• Find time to snack healthily. Take short food breaks to help keep your blood-sugar level reasonably high without surging. Eating a piece of fruit every three hours or so, for example, could prevent hunger and overconsumption of calories. And when you eat, relax. Try not to think about your research. If you routinely stand in the lab, sit down. If your role is more sedentary, get up and take a quick stroll — perhaps to see a colleague on the next floor.
• Put food on your agenda. Schedule regular mealtimes in your work diary — because if you don’t, someone else will fill the gap for you by inviting you to a meeting. Choose a slot that aligns with your ‘biological clock’ and alterations in hormones such as insulin to optimize metabolic health, including microbiota diversity and composition. In other words, follow your gut and eat at times of the day when you feel that your body needs it, but generally try to avoid taking lunch too late in the afternoon. Eating earlier in the day can improve your energy balance, weight regulation, glycaemic control and sleep satisfaction6. Your brain consumes about 20% of the total energy used by your body, so maintaining consistent energy levels is important for optimal functioning. Use the time you’ve booked. Focus on what you eat and take your time. Do not grab a sandwich and munch it down in front of a screen. Your body deserves a rest.
• Enjoy your food. Transform your meal break into a pleasant event by sharing it with colleagues. Propose that everyone take turns preparing a dish from their home country or area so that you can all enjoy the cuisines of different cultures. Eating in a group and discussing the day’s events can help you to relax, to laugh and to share useful information and experiences.
• Plan your meals. If you are feeling particularly hungry, your eyes and hypothalamus (a small region in the brain that controls many bodily functions including hunger and thirst) will not help you to make healthy food choices; instead, they will prompt you to go for sugary, salty or fatty options. Try to organize your meals in advance. Increase your intake of low-calorie items, such as soups, salads, vegetables and minimally processed foods that are rich in dietary fibre. Among these are wholegrains, cereals, fruits, pulses, whole rice and wholemeal pasta. These foods are also rich in micronutrients and antioxidants such as potassium, magnesium, vitamin C, vitamin E, B-vitamins and healthy lipids — especially unsaturated omega-3 ones — that can help to prevent chronic disease. Neurotransmitters such as serotonin, dopamine, epinephrine and norepinephrine — all important for good brain function, mood and emotional regulation — require food-derived precursors, as well as vitamins and minerals, to be synthesized7.
• Diversify your diet. Stimulate your appetite by altering your food choices, preferably by incorporating more fruit and vegetables into your diet and reducing consumption of red meat and meat products. Each new day merits a new meal experience. But this doesn’t mean being a fully fledged connoisseur: overthinking what you eat will lead to compromises with your time and will make further compromises in what you eat more tempting. A saying from the Japanese Okinawa islands, where people have one of the lowest rates of chronic diseases in the world, and where many centenarians live, points the way: “Eat until you are 80% full”8. In practice, this means you should eat slowly and avoid ‘stuffing’ yourself.
• Avoid the insulin roller coaster. As well as contributing to chronic disease, excessive sugar intake might harm cognitive performance9. Sugared drinks, such as sodas, smoothies and even fruit juices, have a very low satiety value. After the sugar surge, glucagon — a hormone produced when sugar levels are low — as well as ghrelin, an appetitive hormone, and others kick back in and you’ll be hypoglycaemic and feel hungry again. Artificially sweetened beverages might not work much better — there is scientific debate about their perceived health benefits, because they might stimulate appetite centrally in the hypothalamus, rather than by modulating insulin levels10. Go for water, coffee, teas (including fruit teas), low-fat milk — or, if you’re desperate for sugar, a homemade fruit juice.
• Drink loads of water. Working inside, where the air is often dry (owing to heating in winter and artificial cooling in summer) can hasten water loss through respiration. Two litres a day of fluid intake is recommended by many health agencies. Pay attention to signs of dehydration. Drinking plenty will increase your blood volume and brain tissue fluid and thus boost your circulation and concentration levels. You will also become more tolerant of heat and cold — which is helpful when working in warm offices and cooled labs. Water is the essential carrier for all life functions in your body. It can also increase daily energy expenditure and feelings of satiety. Drinking water half an hour before your meal is an especially good option because it improves satiety11.
• Use healthy leftovers. Pre-packaged sandwiches and processed foods often have high quantities of fat, sugar, salt and additives that trigger the brain’s dopamine reward system, among other neuronal systems, inducing compulsive eating behaviour12. If you have time, prepare a healthy dish from scratch at home, perhaps making more than is needed for an evening meal and using leftovers for lunch the following day. Among homemade foods, well-balanced traditional dishes can improve your performance and health: for instance, the classic Mediterranean diet has long been linked with improved cognitive function and a decreased likelihood of both cognitive impairment and Alzheimer’s disease3. A Tupperware lunch made with leftovers from even the most indulgent dinner could often make a healthier lunch than a standard pre-packaged sandwich.
• Scrap the salt. Excessive use of salt is among the major killers worldwide, leading to increased blood pressure, stroke and other cardiovascular diseases. Some salt is essential to the taste of most foods, as well as for life, however, so don’t attempt to cut it out of your diet entirely. Try pepper, curcuma, nutmeg or other spices to add flavour. Some spices, including curcuma and pepper, also help to lower the risk of cardiovascular disease and can even decrease total mortality rates13.
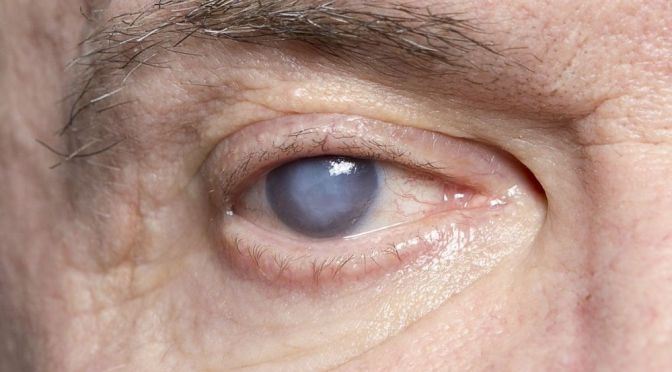
Eye Health: Cataracts
Cataracts involve the lens of the eye which is located just back of the cornea.
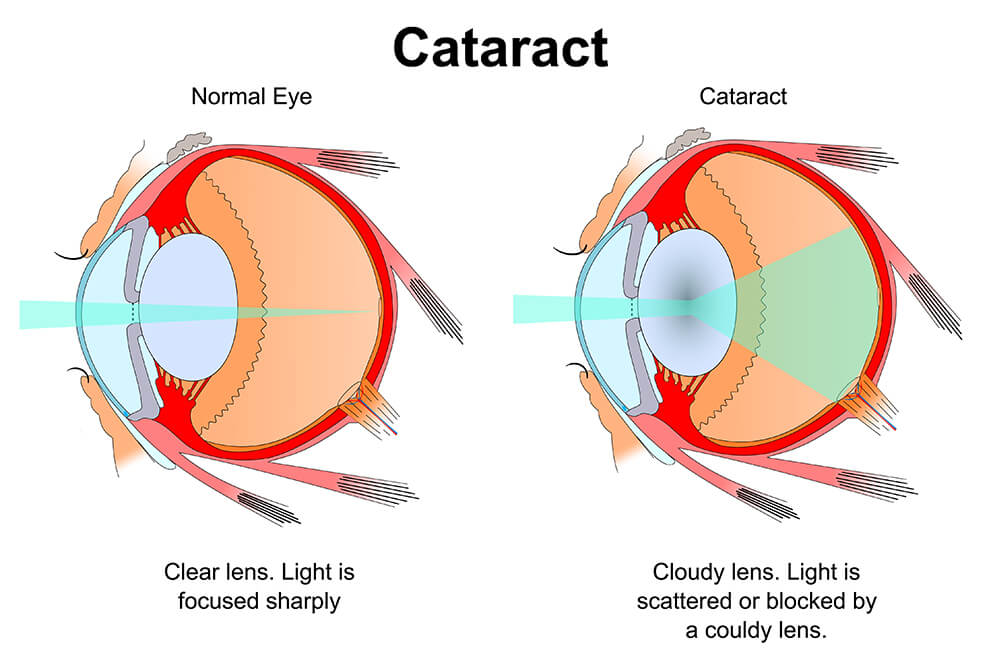
The lens is composed of evenly aligned collagen fibers which are progressively damaged by ultraviolet light as we age. Cataracts cause clouding of the lens and reduce visual acuity, as well as causing a stiffening and rigidity of the lens which keeps it from changing shape for close-up activities like reading.
If you live long enough, cataracts are almost inevitable and the main decision is when to get them corrected. With intraocular lenses, the operation has few downsides.
The halo around oncoming headlights disturbed my night driving, and was a major reason for me to get my cataracts removed.
I used to require glasses all the time, and took them off to read. Now I wear no glasses, and even reading is possible without glasses, since one of my eyes has a -1.5 diopter cylindrical astigmatism. You can ask for one Intraocular lens to be slightly nearsighted, if you wish to avoid needing reading glasses.
I prefer to use my corrective glasses to read, however.
—Dr. C.
DOCTORS PODCAST: MEDICAL & TELEHEALTH NEWS (MAR 20)
A weekly podcast on the latest medical, science and telehealth news.
Shoulder Pain: Rotator Cuff Repair (Mayo Clinic)
Diagnosis: Six Warning Signs Of Colon Cancer
Colon cancer is one of the most common cancers in people of all genders and the third leading cause of cancer-related deaths in the United States. It happens when the cells that line the colon become abnormal and grow out of control.
Chapters: 0:00 Intro 0:22 What is colon cancer? 1:00 6 warning signs of colon cancer 2:13 How are patients screen for colon cancer? 2:32 Who is at risk for colon cancer? 3:15 Is colon cancer treatable?
Skin Conditions: What Are The Causes Of Rosacea?
- Alcohol. Alcohol can dilate the tiny blood vessels in the face, causing the face to flush. Drink in moderation only on special occasions, if at all. Not only can drinking alcoholic beverages cause flare-ups, but so can topically applied alcohol in various facial cleansing products. Always check product ingredients and avoid those containing alcohol or other overly drying ingredients.
- Spicy or hot foods and drinks. Foods that contain spicy ingredients can affect the blushing areas of the face, leading to redness. If you love spicy food, go with mild spice and only enjoy these dishes on occasion. Since hot (temperature-wise) food and drinks often trigger facial flushing, you should allow your food or warm beverage to cool a bit before consuming.
- Exercise. Regular exercise is important for everyone, but it’s also a common trigger for rosacea flare-ups. But don’t abandon your exercise routine. Rather, limit outdoor exercising to morning or evening hours to avoid midday heat and sun exposure. When exercising outdoors, use shaded trails for cycling or jogging. And always remember to keep yourself well hydrated.
- Sun and wind exposure. Sun exposure, hot and cold temperatures and wind exposure frequently aggravate rosacea symptoms. Always wear a broad spectrum sunscreen when outside, even on cloudy days. If possible, stay inside on particularly hot, humid days. If you must venture out in the cold or wind, cover your cheeks and nose with a scarf.
- Anxiety and stress. Stress and anxiety can cause rosacea symptoms to worsen, so use stress management techniques when needed. Make sure to get plenty of rest and practice deep breathing when you feel anxiety creeping up.