I started having hand pain about 20 years ago, and booked a visit with the rheumatologist in my medical building. He looked at my hands and immediately knew that I had osteoarthritis.
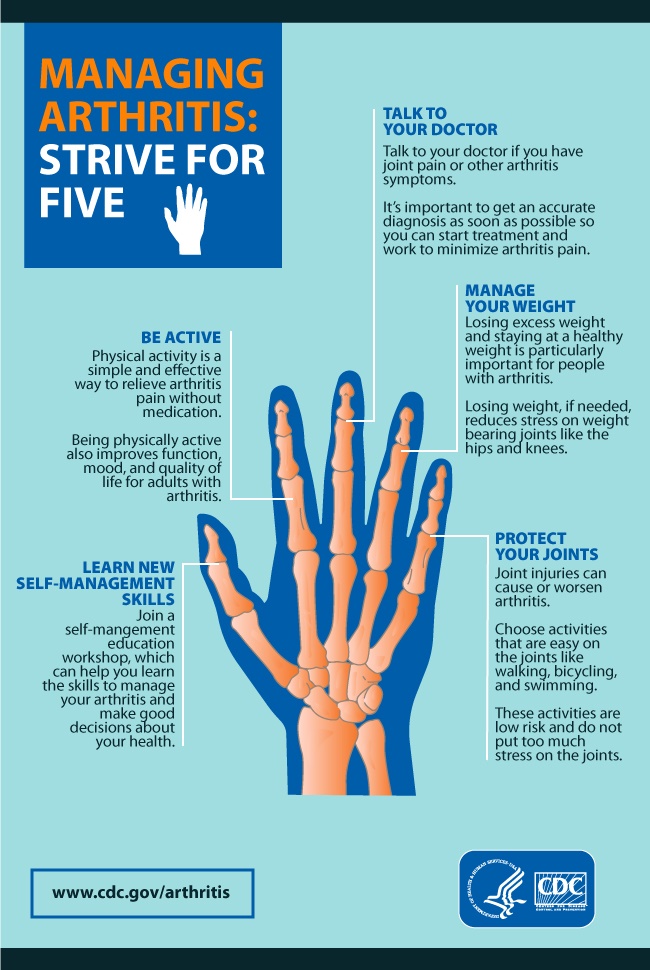
The thumb musculature (the thenar eminence) was angled with respect to the plane of the rest of my hand and wasn’t flat like normal. Some of my joints were slightly swollen and even warm to the touch, and many of my fingers were beginning to get crooked.
He ordered a rheumatoid panel, uric acid and inflammatory markers. The normal results confirmed his diagnosis of osteoarthritis.
The middle and index fingers have taken a lot of trauma over the years. They are also the crookedest, for the same reason. With the thinning of my skin or you can see the outline of my tendons on the palm of my hand, and some are a little bit bumpy and irregular. I am unable to make a tight fist anymore, although my fingers will flex to some degree.
I practice exercises on my wrist, hands and fingers, such as rotating my wrist and thumb in a circular fashion, touching my thumb to the tips of my fingers in sequence, squeezing a rubber ball, and flattening out my hand against the back of my head. Recently, I have noticed a little resistance when I try to straighten out my ring fingers after flexing them, and worried about developing trigger finger. On further reading I found that trigger finger is not more common in people who have osteoarthritis.
I do a lot of swimming, and am worried that the irritative force of the water regularly acting up on my hand might be making the hand pain worse. But my hands seem to be a little bit better with the hand exercises. There seems to be less pain, although maybe I have the same amount of pain but tolerate it better since I’m doing something about it. One never knows about a preventative program, since you’re an experiment of one. You have to have faith that what you are doing is beneficial, and in harmony with medical studies. Perhaps my anti-inflammatory diet and turmeric, as well as my good sleep and aerobic exercise is also helping.
—Dr. C.