Exercise training is a safe, effective and low-cost intervention for improving walking ability in patients with IC. Additional benefits may include improvements in QoL, muscle strength and cardiorespiratory fitness. Clinical guidelines advocate supervised exercise training as a primary therapy for IC, with walking as the primary modality.
However, evidence is emerging for the role of various other modes of exercise including cycling and progressive resistance training to supplement walking training. In addition, there is emerging evidence for home-based exercise programmes. Revascularisation or drug treatment options should only be considered in patients if exercise training provides insufficient symptomatic relief.
Abstract
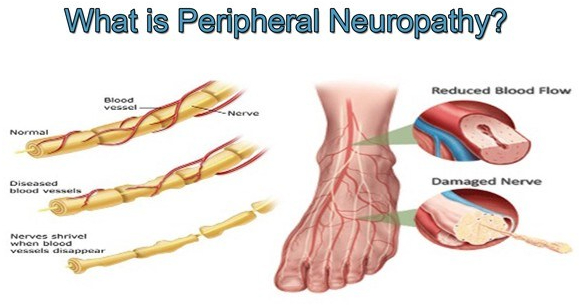
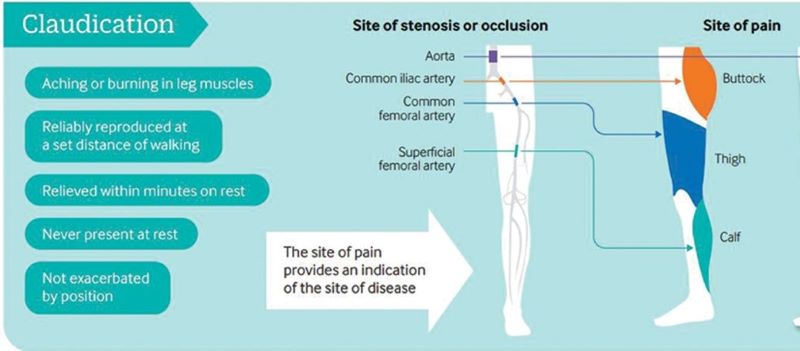
Peripheral artery disease (PAD) is caused by atherosclerotic narrowing of the arteries supplying the lower limbs often resulting in intermittent claudication, evident as pain or cramping while walking. Supervised exercise training elicits clinically meaningful benefits in walking ability and quality of life. Walking is the modality of exercise with the strongest evidence and is recommended in several national and international guidelines. Alternate forms of exercise such as upper- or lower-body cycling may be used, if required by certain patients, although there is less evidence for these types of programmes. The evidence for progressive resistance training is growing and patients can also engage in strength-based training alongside a walking programme. For those unable to attend a supervised class (strongest evidence), home-based or ‘self-facilitated’ exercise programmes are known to improve walking distance when compared to simple advice. All exercise programmes, independent of the mode of delivery, should be progressive and individually prescribed where possible, considering disease severity, comorbidities and initial exercise capacity. All patients should aim to accumulate at least 30 min of aerobic activity, at least three times a week, for at least 3 months, ideally in the form of walking exercise to near-maximal claudication pain.