Sleep apnea and obesity are bound together as Charles dickens observed in his Pickwick papers. The Pickwickian syndrome is obesity associated with alveolar hypoventilation(insufficient breathing) with an increase in CO2 in the bloodstream which causes narcosis, or SLEEPINESS, in the daytime.
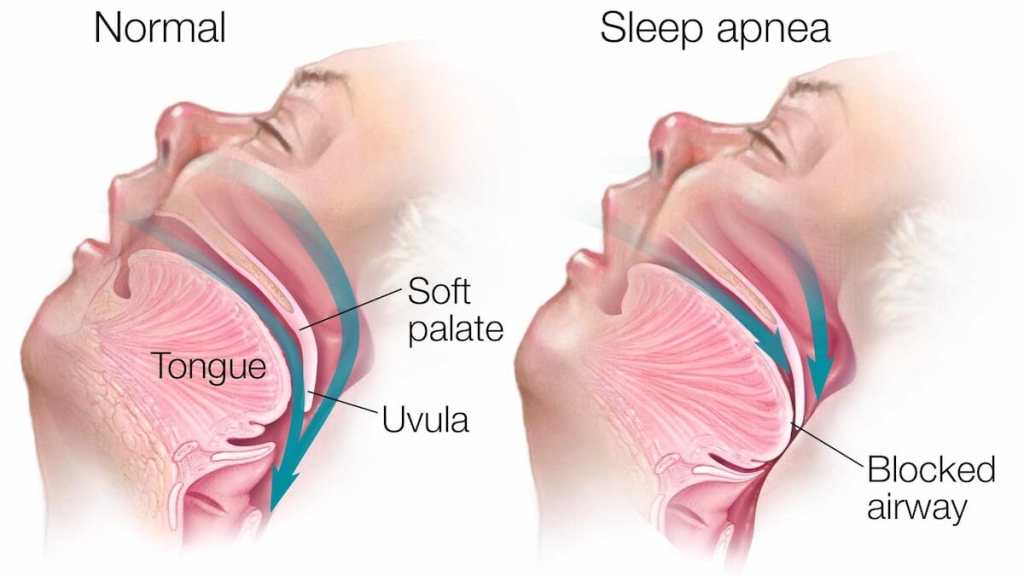
When I went in for my sleep apnea study, I noticed a number of double wide chairs available for the usual clientele there. OBESITY is one of the major risk factors for sleep apnea. Depositions at the base of the tongue and throat interfere with breathing, and causes snoring to the point of tracheal blockage and apnea at night.
Some people with normal “ BMI”, have sleep apnea. Sleep apnea can run in families, occur when you are older, or have a thick neck. So no matter what your weight, if you have daytime sleepiness after an apparently full night of sleep, you should be considered for a sleep study.
A SLEEP STUDY requires that you go into a sleep center overnight, get hooked up to an electroencephalogram machine, oxygen monitor, chest straps, and the like. This is the gold standard for a diagnosis of sleep apnea, but a recording pulse oximeter will let you know a lot less expensively if you have the critical problem, a drop in oxygen saturation. The type of sleep apnea I have been discussing so far is obstructive sleep apnea. Of course there are other types such as central, or complex sleep apnea.
Most sleep apnea responds to nasal CPAP, if you can tolerate it.
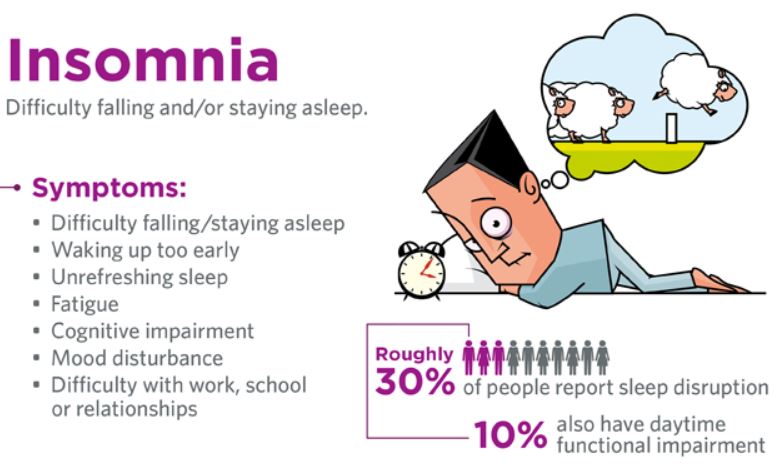
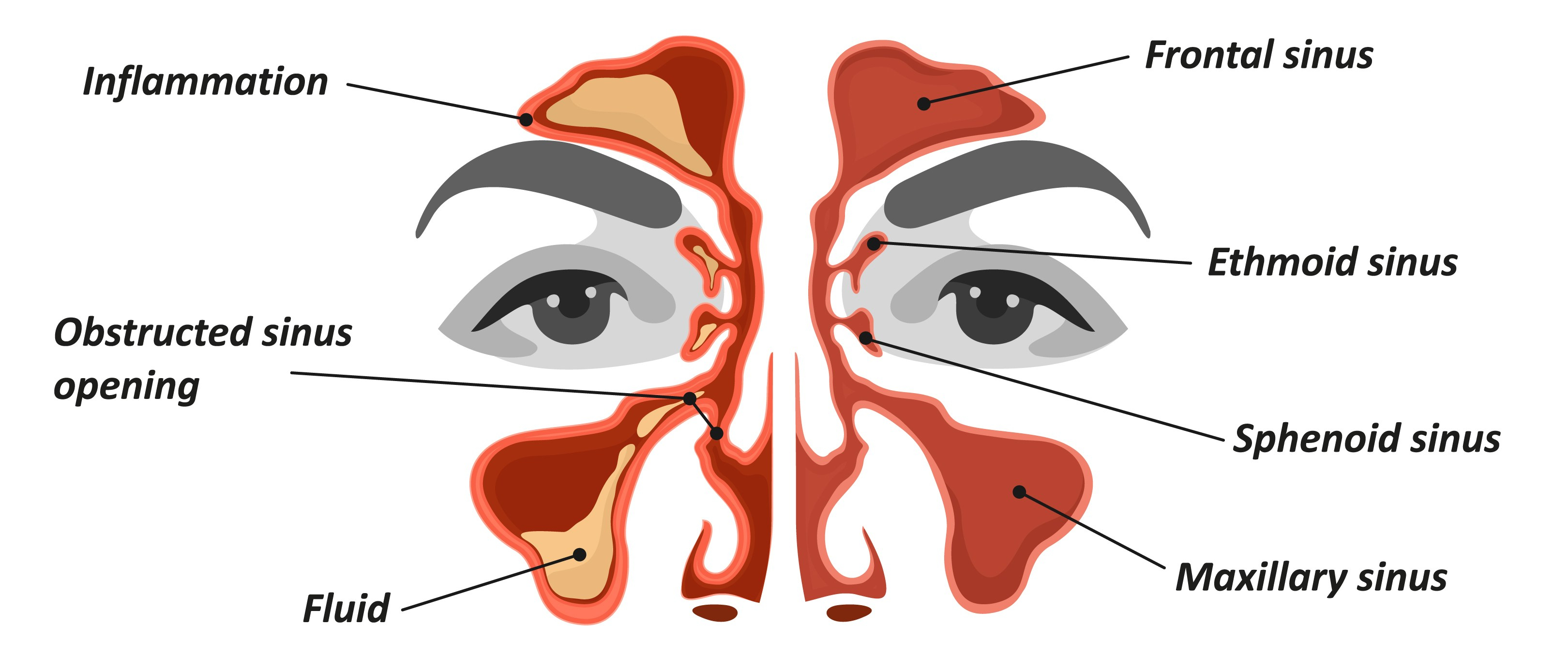
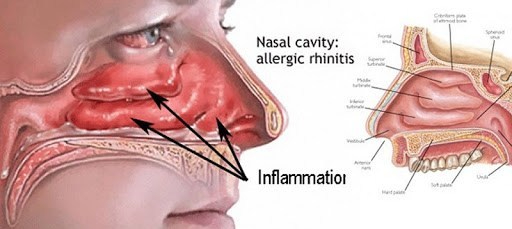
My own sleep apnea was diagnosed as moderate, 15% central and 85% obstructive in type. I have a stuffy nose which I believe to be the main problem setting me up for sleep apnea, and I could not tolerate the positive nasal CPAP. There is also a dental apparatus that I tried unsuccessfully. I wound up sleeping on my side, and propping myself in that position with pillows .This seems to help me, but I still wake up several times a night, usually at the end of a 90 minute sleep cycle, and with a full bladder.
I sleep through better on days when I have had more physical or mental exercise. Avoiding a full stomach at bedtime is also helpful with both sleep apnea and GERD.
I do use Afrin on the left side of my nose, which is more obstructed. I restrict the use to every third day, although I have heard that you can use it every other day, alternating sides, if you have a stuffy nose that has resisted other treatments .I have also heard that using corticosteroid nasal sprays makes Afrin better tolerated. Be sure to get clearance with your doctor before trying this.