These are four of the most common tests for inflammation:
- Erythrocyte sedimentation rate (sed rate or ESR). This test measures how fast red blood cells settle to the bottom of a vertical tube of blood. When inflammation is present the red blood cells fall faster, as higher amounts of proteins in the blood make those cells clump together. While ranges vary by lab, a normal result is typically 20 mm/hr or less, while a value over 100 mm/hr is quite high.
- C-reactive protein (CRP). This protein made in the liver tends to rise when inflammation is present. A normal value is less than 3 mg/L. A value over 3 mg/L is often used to identify an increased risk of cardiovascular disease, but bodywide inflammation can make CRP rise to 100 mg/L or more.
- Ferritin. This is a blood protein that reflects the amount of iron stored in the body. It’s most often ordered to evaluate whether an anemic person is iron-deficient, in which case ferritin levels are low. Or, if there is too much iron in the body, ferritin levels may be high. But ferritin levels also rise when inflammation is present. Normal results vary by lab and tend to be a bit higher in men, but a typical normal range is 20 to 200 mcg/L.
- Fibrinogen. While this protein is most commonly measured to evaluate the status of the blood clotting system, its levels tend to rise when inflammation is present. A normal fibrinogen level is 200 to 400 mg/dL.
Commentary:
Inflammation is an essential, evolutionarily conserved mechanism that our bodies have developed for excluding infections, toxins, and damaged or cancerous cells.
Acute inflammation in response to infections is almost always beneficial, except where it is disproportionate to the danger that it fights; the common cold is probably innocuous, but we develop symptoms from our bodies’ response. Covid has been found to incite disproportionately severe inflammation, which can lead to severe disease, and the need for corticosteroids.
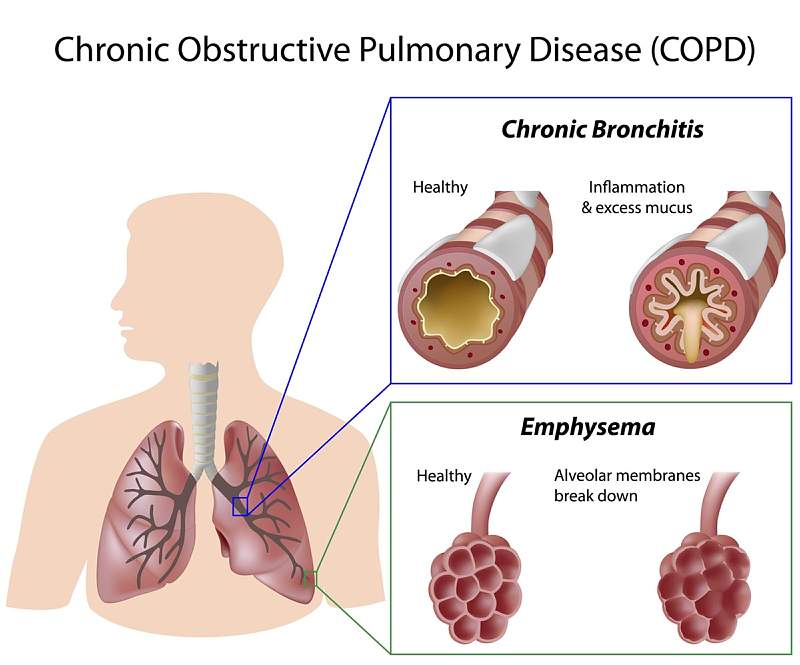
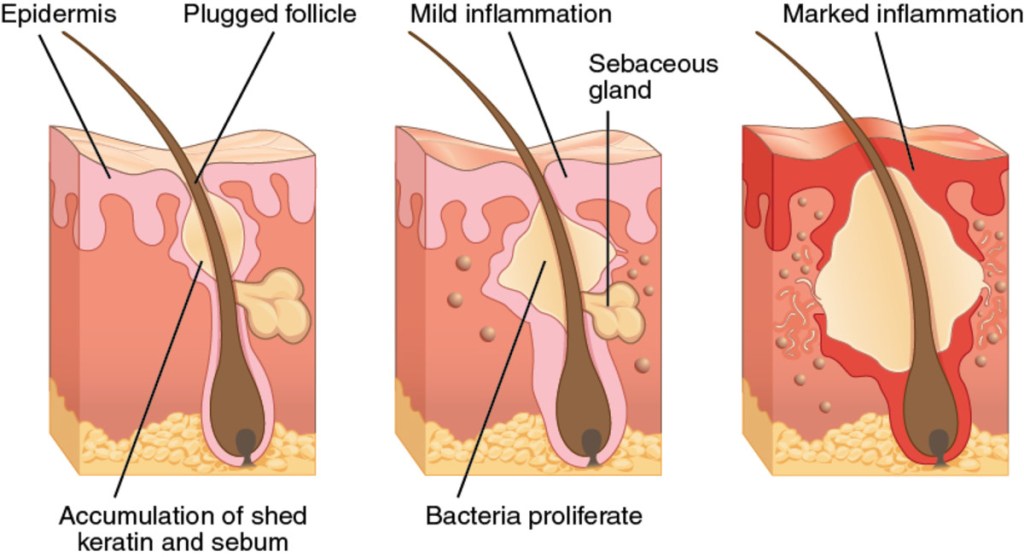
Chronic inflammation is a different animal, and is usually undesirable. Sometimes it is due to an infection, such as tuberculosis, which won’t go away. Sometimes the bodies immune system develops a disordered communication system, and fights its own cells, called auto immunity.
Chronic inflammation can also be caused by obesity, chronic stress, cigarette smoking, alcohol in excess, and cancer, which can also be CAUSED BY chronic inflammation.
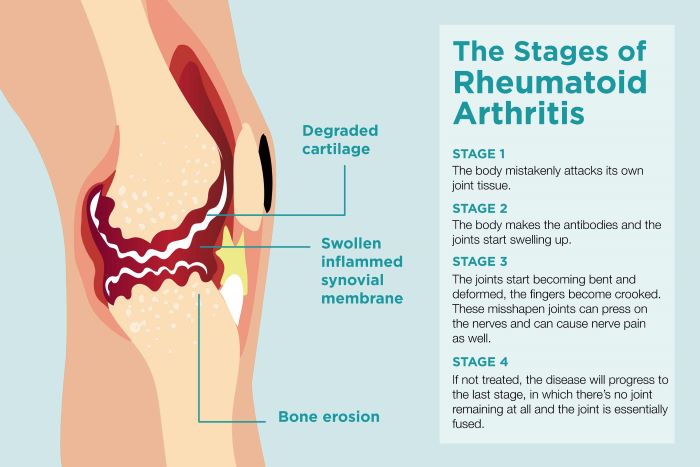
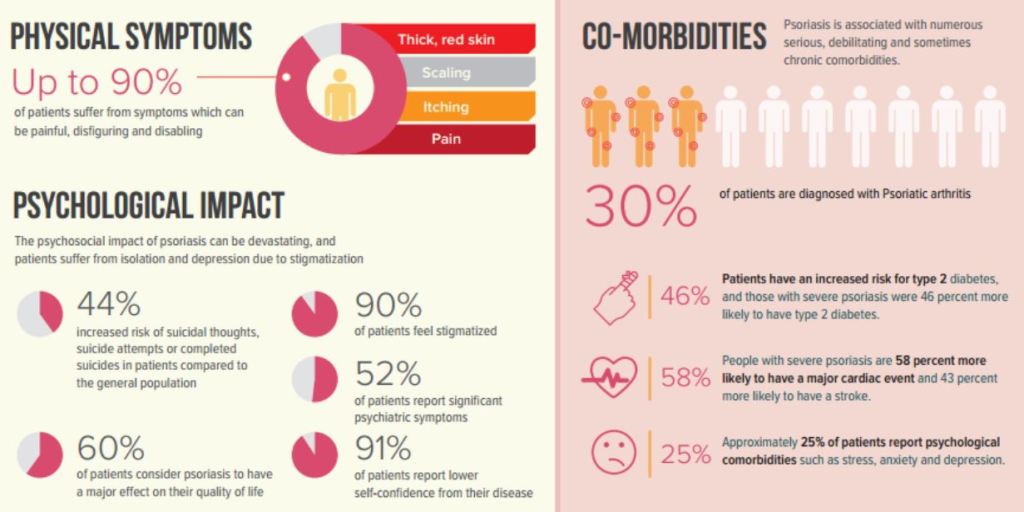
Chronic inflammation is also associated with Alzheimer’s, heart disease, rheumatoid arthritis, and type two diabetes. Asthma is a chronic inflammatory disease of the airways. IBD, inflammatory bowel disease, is a chronic inflammatory disease of the intestinal tract.
The symptoms of chronic inflammation very widely depending on the area involved. Abdominal pain, chest pain, joint pain, skin rashes, fatigue, and fever are some of the symptoms.
You can reduce your likelihood of chronic inflammation by maintaining normal weight, having regular exercise, eating a diet rich in natural vegetables and fruits (antioxidants), avoiding alcohol and cigarette smoke, and by reducing or handling your stress.
—Dr. C.