Old age is an inevitable condition if you are lucky enough to live a long life. Middle aged people say it begins at 70 years of age. According to an Elysium survey of people 40 and older, the average American FEELS old for the first time at age 47 years.
In the distant past, 50 was CONSIDERED to be old. The generally better conditions and Medicine of modern times keeps extending LIFESPAN, if not always HEALTHSPAN. Old age is certainly a Condition, and it is for sure Chronic, thereby qualifying for inclusion, but is it a Disease?
It is not considered a disease by the authorities, and so it doesn’t gather research funds like it should. What exactly IS old age? Being 88 Years old, and a physician, I feel qualified to comment. Old age is a collection of past accidents and sports injuries plus complications of past illnesses engrafted on a gradually deteriorating body.
Where does Obesity and Metabolic syndrome fit in this rubric? The Plague of our time fits in the disease category. It is definitely preventable, although with difficulty. Please search past postings for more information on this topic.
In what way does the body gradually deteriorate? Any organized, non-random high information structure gradually becomes more disordered, and “worn away” with the passage of TIME, the destroyer. Entropy (disorder) gradually increases, in the absence of corrective energy input.
Even rocks and mountains eventually erode, given enough time. One of the most interesting characteristics of life is that it maintains its integrity for an inordinate amount of time, given its complexity and furious dynamism.
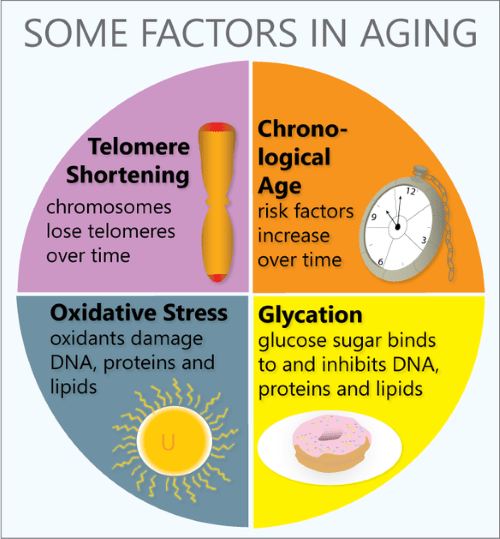
Every day our DNA sustains thousands of molecular ruptures from high energy radiation and other stressors. Proofreading and repair mechanisms are employed, at high energy cost, to repair these breaks. This corrective is especially efficient when we are young and vigorous; In our youth, our reproductive years, growth and repair predominate. Gradually, growth ceases, repair mechanisms age, and we become old.
Our Darwinian “warranty” expires. We are left with an aging body, unimportant to evolution. We are long on experience and short on future. But we still have a marvelous metabolism at our disposal, depending on our lifestyle. There are a number of metabolic pathways which affect aging, 2 of which have been more studied.
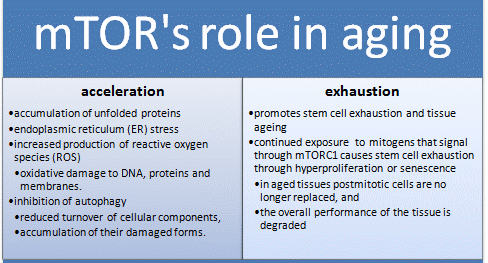
The mTOR pathway is most attuned to youth, senses nutrients and gears up for ANABOLISM, or growth. If you have not been careful to tailor your food intake to suit your decreasing requirements, your efficient metabolism stores it away for a rainy day, around your belly and in your arteries, a bad effect from an essential mechanism. Antagonistic Pleiotropy is the name for a body mechanism that can be good for one function (or age) and bad for another.
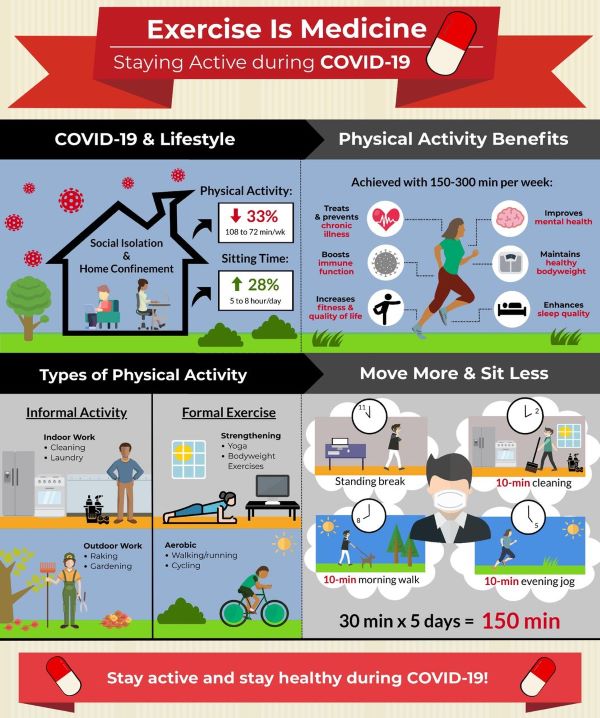
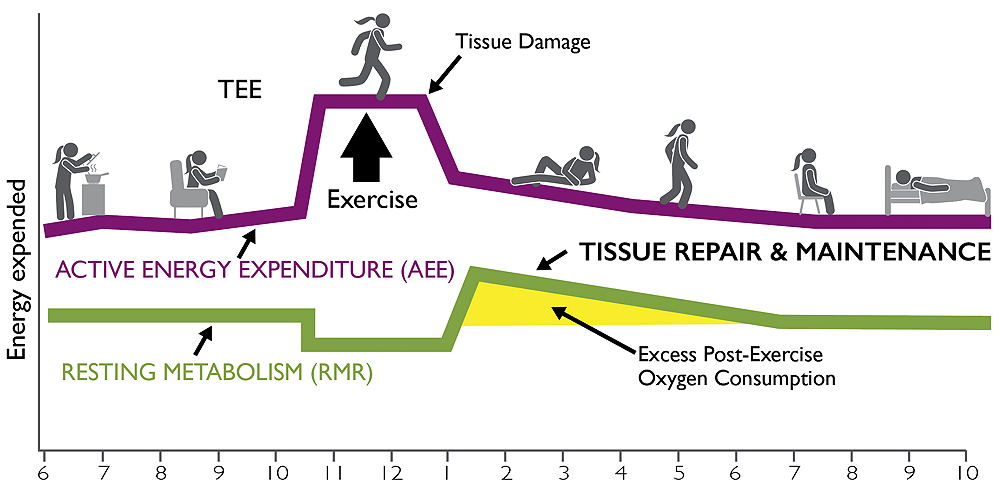
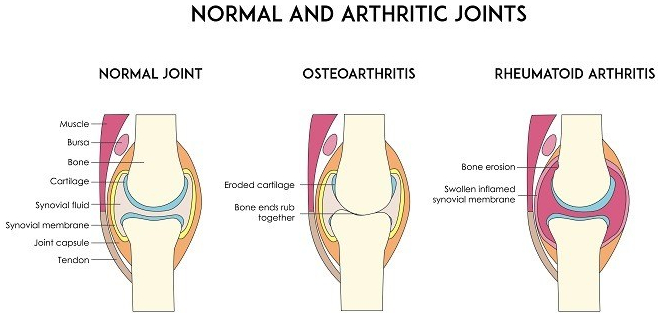
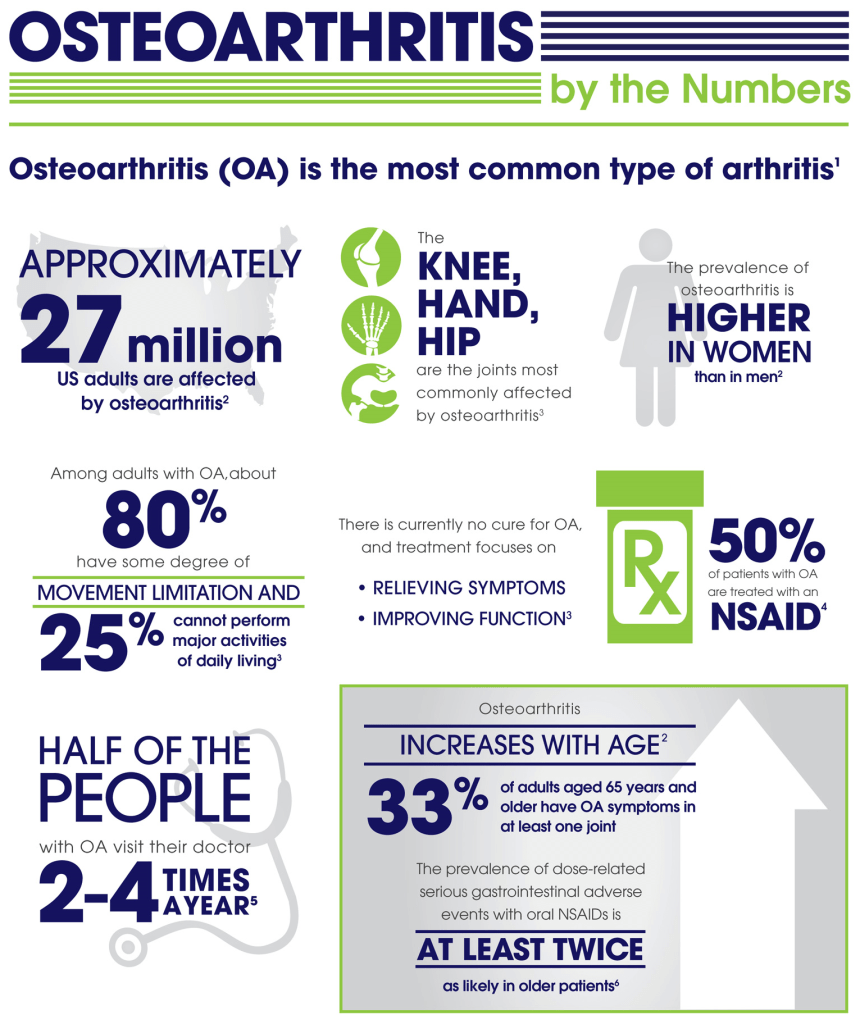
The Sirtuin system is also important in aging, and has a variety of housekeeping functions, including mitochondrial maintenance. It is activated by exercise. The cells of our bodies change with aging. In old tissues, there are less stem cells and other young, functional units. There are more damaged, dysfunctional “zombie” cells that don’t do much but promote inflammation, and hence more inflammatory cells accumulate.
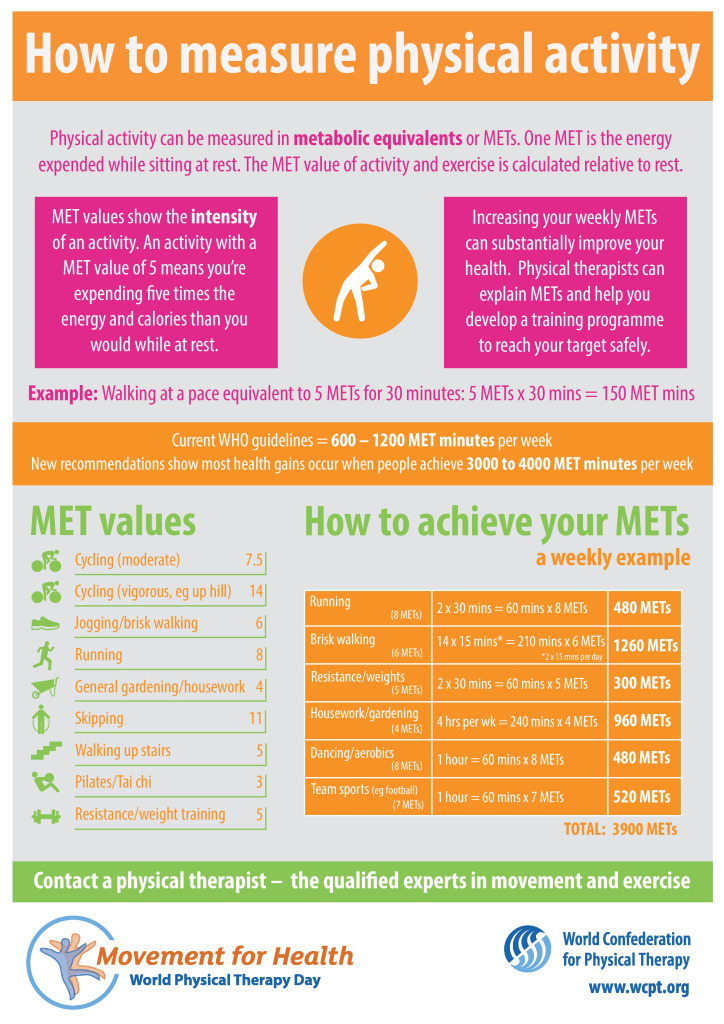
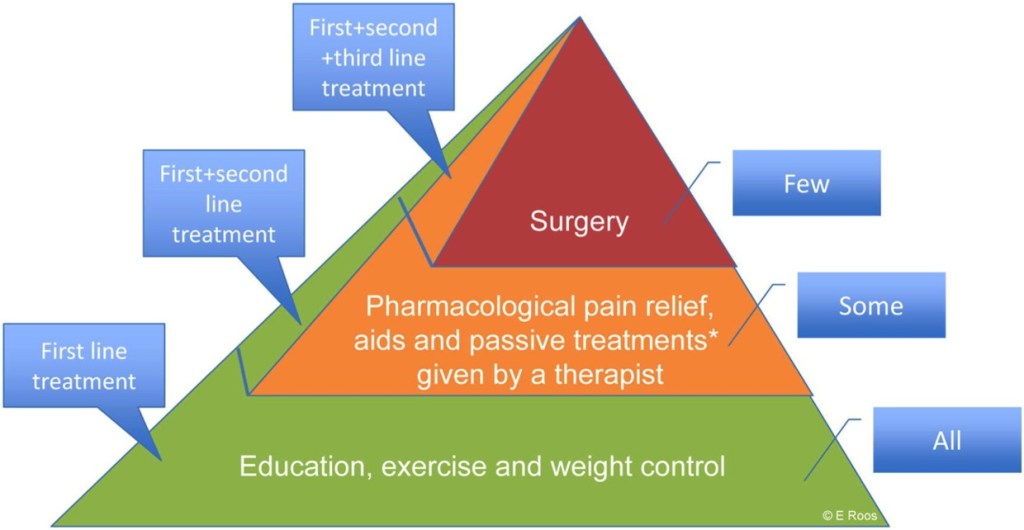
Controlling the mTOR System and promoting the sirtuins help increase apoptosis and get rid of dysfunctional cells, including cancer. DOCTORS SHOULD PRESCRIBE EXERCISE, as well as SLEEP AND DIET, like they do medicine, and maybe we wouldn’t need so many pills. We might also feel better into old age.
–Dr. C.
Disease, Metabolic syndrome, Entropy, DNA, Metabolism, Apoptosis, Zombie cells