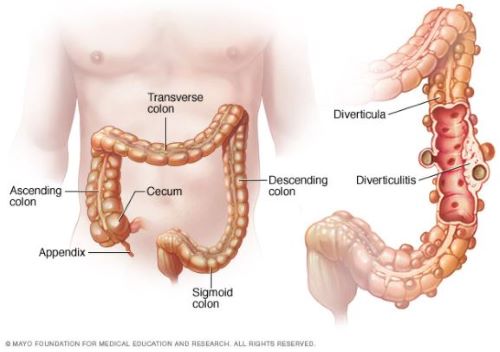
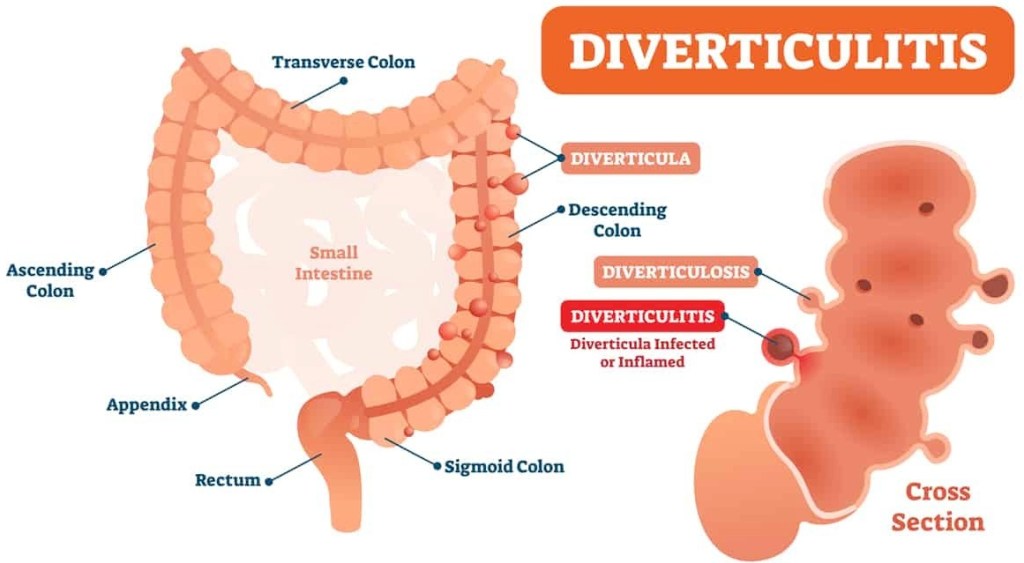
What is diverticulitis?
Diverticulitis arises from a condition called diverticulosis, which occurs when weak areas in the inner wall of the colon bulge outward and form tiny pouches. Many people get diverticulosis as they age. In fact, diverticulosis affects about 58% of US adults over age 60. Getting enough fiber in your diet can help protect against diverticulosis.
Know the signs of diverticulitis
The most common symptoms of diverticulitis are abdominal pain (usually on the lower left side) and fever. The pain is distinct and sharp, and may strike over a few hours. Other symptoms may include a combination of loss of appetite, nausea, vomiting, abdominal bloating and cramping, and not passing gas or stool.
A mild case of diverticulitis that causes only minimal pain in the lower abdomen can resolve on its own within a day or two. However, you should seek immediate medical attention if your symptoms are not going away or you are feeling worse, such as having increasing pain, fever, bloody stools, or abdominal bloating with vomiting.
Treatment depends on whether you have uncomplicated or complicated diverticulitis. Your doctor can determine this by using a combination of blood tests and imaging studies, such as a CT scan.
How is uncomplicated diverticulitis treated?
As the name implies, uncomplicated diverticulitis is the less serious of the two. It means that the inflammation or infection is confined to one section of the colon, and that there is no evidence of complicating factors.
Uncomplicated diverticulitis is typically treated at home with oral antibiotics. You’ll also be prescribed “bowel rest” for a few days, which often includes a clear liquid diet. This gives your bowel a chance to rest and heal, and may reduce pain. Additionally, you’ll follow a low-fiber diet (about 10 to 15 grams of fiber a day) until your symptoms improve.
Some people may need to be hospitalized to receive intravenous (IV) antibiotics. A hospital stay is more likely if you’re 65 or older or have other medical conditions, such as heart disease, diabetes, or chronic obstructive pulmonary disease.
People usually begin to feel improvement from treatment after about three days. If you feel well enough and the symptoms have subsided, you can gradually resume your regular diet.
If symptoms haven’t responded to antibiotics after a week, you probably will undergo CT scans and other tests to see if you have complicated diverticulitis.
How is complicated diverticulitis treated?
Complicated diverticulitis means you have a specific complication that requires a longer course of IV antibiotics, and possibly surgery.
Pope Francis had scarring in a segment of colon where he previously had diverticulitis, which had caused a narrowing in the colon called stenosis. In a case like this, the unhealthy part of the colon is removed, and the remaining colon is then reconnected.
Other types of complications that may occur during an active diverticulitis infection include:
- Abscess. A diverticular abscess is a collection of pus (a fluid that can form at the site of infection) outside of the intestinal wall. If the abscess doesn’t get better with antibiotics, a doctor will need to drain the pus using a needle, under guidance through images on a CT scan.
- Perforation. Diverticulitis can cause a hole in the colon that allows bowel contents to spill into the abdominal cavity. If you have a perforation, your abdomen may feel tender to touch, hard, or enlarged. Surgery repairs the hole. Sometimes part of the colon around the hole must be removed.
- Fistula. A fistula is an abnormal connection between the inflamed and infected segment of the colon and adjacent organs, such as other parts of the intestine or the bladder. Surgery consists of colon resection and removing the fistula.
Can diverticulitis be prevented?
Eating a high-fiber diet and managing stress may lower the risk of developing pouches in the colon known as diverticula. So it makes sense that these lifestyle interventions might help make diverticulitis less likely to occur. However, once you have diverticulosis, there is no proven way to prevent one of the diverticula from becoming infected or inflamed.
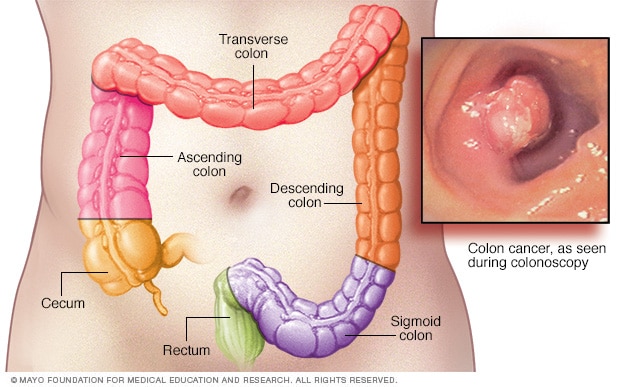
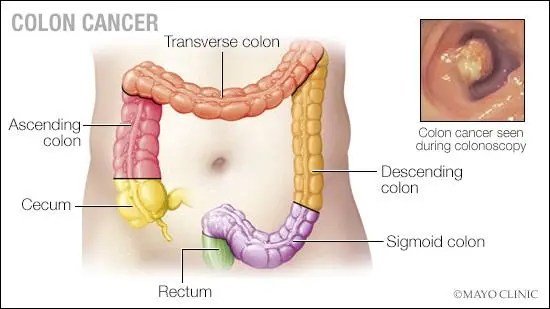
Mayo Clinic Cancer Blog – Colon cancer can occur in any part of the colon. An examination of your entire colon using a long, flexible tube equipped with a camera (colonoscopy) is one way to detect colon cancer and polyps. It can be easy to feel confused by screening recommendations for common types of cancer. Test your knowledge of why, when and how you can be screened with these myths and facts: