During the holiday season, it can be hard to pass on that extra piece of pie. Learn about the science of hunger. #HealthyEating https://t.co/RACMyq5kJn
— Northwestern Medicine (@NorthwesternMed) December 24, 2021


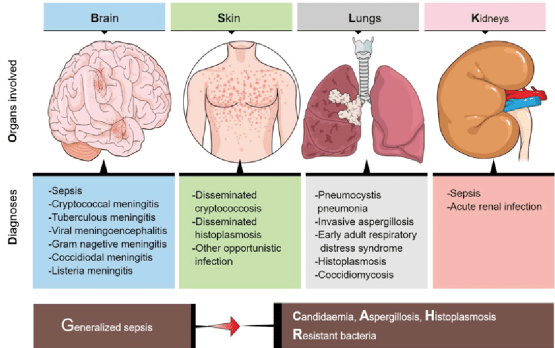
Cryptococcus neoformans and gattii are fungi that most commonly infect people with immunodeficiency, especially AIDS, which is highly prevalent in Africa. Cryptococcus is the final cause of death in perhaps 25% of AIDS patients and preventative treatment is sometimes used if the lymphocyte count is too low.
It is an opportunistic fungus, with similarities to pneumocystis carina, which is discussed in a previous entry.

The areas in the body most commonly affected are the lungs, the skin, and the brain. The lung and skin, being exposed to the environment, are the most common entry points for the fungus, and the brain is a frequently involved area. Chronic meningitis, where the symptoms include headache, blurred vision, and confusion, is frequently caused by cryptococcus.
Sometimes, in healthy people, the skin can be infected with “pigeon breeders disease”. Pigeon droppings are a very common source of cryptococcus organisms.
Infection In the lung is usually restricted to immunocompromised individuals, who develop cough, shortness of breath, and fever. Pulmonary cryptococcosis is a slowly developing disease, can be mistaken for tuberculosis, and frequently gets into the bloodstream and then into the brain.
Treatment is usually with amphotericin B and flucytosine.
Read more
Fungi are in the outside air, the inside air, and even the air of isolation units In hospitals. The normal human respiratory tract is able to breathe these fungi in, have them deposited on the mucous membrane surfaces and have no problem. The normal respiratory membranes, with their associated cleansing cilia and normal mucus production are able to sweep the invaders out without sustaining any harm.
Problems arise when the respiratory tract is functionally or structurally abnormal, such as in cystic fibrosis, bronchiectasis and COPD. Immunocompromised conditions have been increasing in frequency with the improvement in medical care in recent years. Intravascular catheters and sensors can provide a resting place for pathogens including fungi, as can cavities, scars and other damage to the lung. The immune system may require suppression to accommodate an organ transplants or ameliorate autoimmune conditions.
Cancers, especially of the hematologic or lymphatic system, such as lymphomas, pose a definite problem. Severe burns and malnutrition may weaken the immune system, as may Viral infections, especially AIDS, and more recently COVID-19. More subtle immune problems may arise with diabetes, Obesity, or even a lack of sleep and exercise.
These and other conditions give the fungal infections the OPPORTUNITY to invade the body, and a few dozen of the thousands of species of fungi proceed to do just that. Opportunistic fungi often have special features, depending upon the species. Most prefer the respiratory tract, and if they get in to the bloodstream can go to their favored spots.
Aspergillus, and coccidiomycosis , for instance, prefer the lung. Mucormycosis often involves the sinuses and eyes. Blastomycosis can involve bone. Sporothrix is often found infecting the skin.
Symptoms depend upon the area involved. Of course if it’s a respiratory tract, you have coughing, mucus production, sometimes shortness of breath. With the central nervous system you have headache and confusion. You can see the involvement in the skin.
The number of drugs available to fight fungal infection is fairly limited, and currently involves only three different classes. Many fungi are resistant to one or two of these classes, and can be problematic.
However, fungi do not as a rule spread through the air from person to person, and a true epidemic would be unlikely.
For many people, depression turns out to be one of the most disabling illnesses that we have in society. Despite the treatments that we have available, many people are not responding that well. It’s a disorder that can be very disabling in society. It’s also a disorder that has medical consequences.
By understanding the neurobiology of depression we hope to be able more to find the right treatment for the patient suffering from this disease. The current standard of care for the treatment of depression is based on what we call the monoamine deficiency hypothesis. Essentially, presuming that one of three neurotransmitters in the brain is deficient or underactive. But the reality is, there are more than 100 neurotransmitters in the brain. And billions of connections between neurons. So we know that that’s a limited hypothesis. Neurotransmitters can be thought of as the chemical messengers within the brain, it’s what helps one cell in the brain communicate with another, to pass that message along from one brain region to another. For decades, we thought that the primary pathology, the primary cause of depression was some abnormality in these neurotransmitters, specifically serotonin or norepinephrine. However, norepinephrine and serotonin did not seem to be able to account for this cause, or to cause the symptoms of depression in people who had major depression. Instead, the chemical messengers between the nerve cells in the higher centers of the brain, which include glutamate and GABA, were possibilities as alternative causes for the symptoms of depression. When you’re exposed to severe and chronic stress like people experience when they have depression, you lose some of the connections between the nerve cells. The communication in these circuits becomes inefficient and noisy, we think that the loss of these synaptic connections contributes to the biology of depression. There are clear differences between a healthy brain and a depressed brain. And the exciting thing is, when you treat that depression effectively, the brain goes back to looking like a healthy brain, both at the cellular level and at a global scale. It’s critical to understand the neurobiology of depression and how the brain plays a role in that for two main reasons. One, it helps us understand how the disease develops and progresses, and we can start to target treatments based on that. We are in a new era of psychiatry. This is a paradigm shift, away from a model of monoaminergic deficiency to a fuller understanding of the brain as a complex neurochemical organ. All of the research is driven by the imperative to alleviate human suffering. Depression is one of the most substantial contributors to human suffering. The opportunity to make even a tiny dent in that is an incredible opportunity.
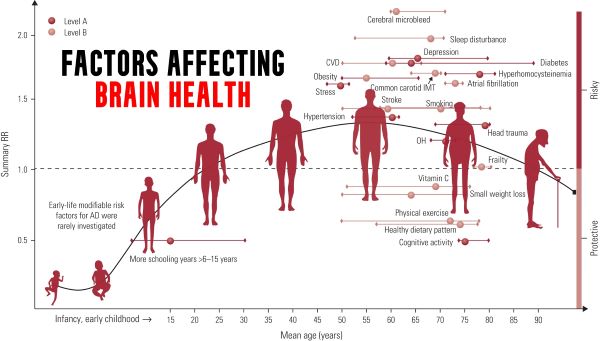
Published online by Cambridge University Press: 22 March 2021
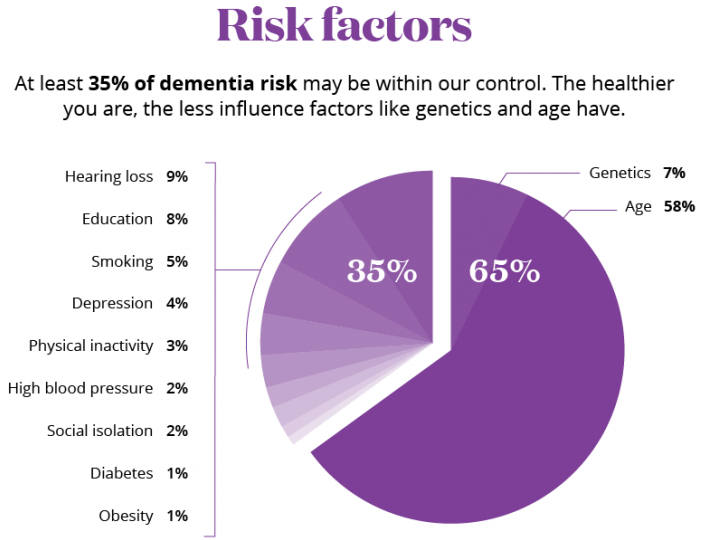
As we age, there are characteristic changes in our thinking, reasoning and memory skills (referred to as cognitive ageing). However, variation between people in the timing and degree of change experienced suggests that a range of factors determine individual cognitive ageing trajectories. This narrative review considers some of the lifestyle factors that might promote (or harm) cognitive health. The focus on lifestyle factors is because these are potentially modifiable by individuals or may be the targets of behavioural or societal interventions. To support that, the review briefly considers people’s beliefs and attitudes about cognitive ageing; the nature and timing of cognitive changes across the lifespan; and the genetic contributions to cognitive ability level and change. In introducing potentially modifiable determinants, a framing that draws evidence derived from epidemiological studies of dementia is provided, before an overview of lifestyle and behavioural predictors of cognitive health, including education and occupation, diet and activity.
We ARE our brains. Reduce the function of any other organ, and we may be sick, but reduce the function of the brain, and WE have changed.
PROGRESSIVE LOSS of brain function is called DEMENTIA. A sudden, temporary (if the cause can be found) is called Delirium. A variety of bad things can cause dementia, such as infections (AIDS), toxins (lead, mercury), chemicals (alcohol), traumatic (CTE from football), diet deficiencies (B12, folic acid), Endocrine deficiencies (thyroid),Psychiatric problems (depression), drugs, and Vascular problems.

The Preceding article on dementia discussed APATHY, as opposed to the somewhat similar DEPRESSION, as a warning sign for SVD, or small blood-vessel disease. SVD is the most common VASCULAR cause of Dementia.
The most common overall cause of Dementia, especially in old age, is ALZHEIMER’S disease (AD). “Senior Moments” are so common as to be a cliche. But this problem is not limited to old age. My 3-year-old Grandson came crying to me that he lost his favorite toy. “Where was it when you last saw it”?, I asked. “It was in my hand” he answered.
He had laid it somewhere, unthinkingly. You can’t remember something unless you ENCODE it. You must be paying attention to, be “mindful” of an action if you are to remember that action.. You will not remember where you put your glasses if you wander around in “default mode”, daydreaming, preoccupied. Everybody occasionally forgets a name, or item which hangs on “the end of my tongue”.
These things, especially “short term memory” do DETERIORATE AS WE GET OLDER. It is common to wonder if we, or a loved one. are getting Alzheimer’s disease, as our mental powers wane.It is often difficult to distinguish the normal forgetfulness of age from DEMENTIA, including Alzheimer’s Disease (AD) It might be a source of REASSURANCE to realize that if you are worried about getting AD YOURSELF, you almost certainly don’t have it; It takes a lot of mental functioning to contemplate that possibility.
Most often, you will be wondering about the possibility in a loved one having AD. There are 2 ideas that I ran across in my reading that might help you do a little evaluation Yourself.
BCGuidelines.ca has a 21 item questionnaire that you can score yourself. 4 points or less is considered normal, so common is forgetfulness. 5-14 points suggests mild cognitive impairment. 15 or more points suggests Dementia, of which AD is the most common type.
The test I really liked was the “Clock Test”. In this test, you draw a large circle. You then ask your loved one to draw a clock, with all the numbers and hands that will indicate 10 minutes after 11. If it is drawn correctly, you can with reasonable certainty EXCLUDE Dementia.
If incorrect, further tests are warranted. I consulted with a Neurologist regarding a friend of mine who has marked memory loss, but is very sweet, is physically capable, takes care of herself personally, doesn’t wander around, has no apparent anxiety, depression or other psychological problems.
I asked if it was reasonable to just watch without any medical intervention. The neurologist said that she should have a blood test, a metabolic panel, TSH (thyroid), LFTs, folic acid and B12 tests, and a CT to rule out NPH (normal pressure hydrocephalus). It is rare to find anything treatable, but a shame to neglect it if present.
If you do see a doctor about a Spouse or Parent with possible dementia, you might request that they discuss the possibilities with you, but ask them not to write the diagnosis of “Alzheimer’s “ in the chart. Private Assisted Living Homes CHARGE A LOT MORE for that Diagnosis– locked facilities, more personnel and the like. BDNF- brain derived neurotrophic factor- can fend off Dementia.
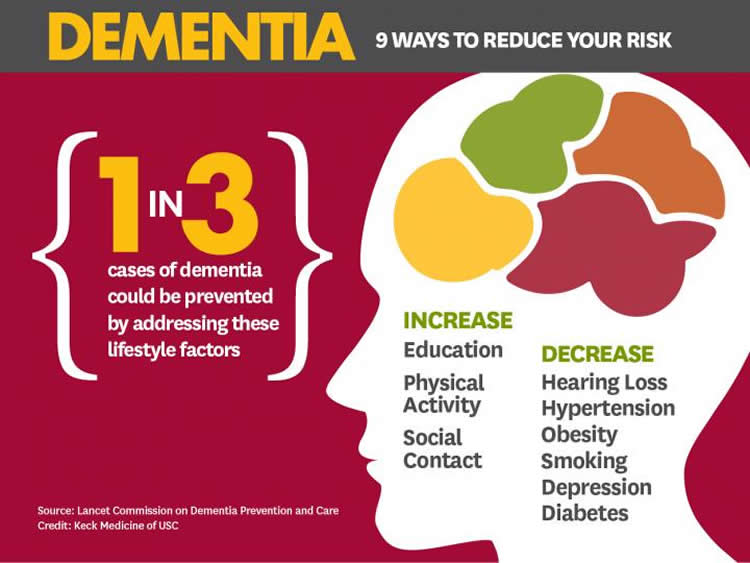
That is the good news. The bad news is that it takes effort and discipline to increase your level od BDNF.; I’m sure medical science is hot on the trail of a pill. But until then, our old friends, Sleep, Diet and Exercise ride to the rescue. Sleep, both N3 and REM stages, increases BDNF. Dietary polyphenols and butyrate increase BDNF. exercise of all kinds will do it.
The BDNF gene codes for the BDNF protein, which promotes the survival, expansion, and differentiation of Neuronal stem cells, and promotes neuronal PLASTICITY, neuronal response to experience. Grit your teeth and develop the HABIT of exposing your Postmodern Body to 3 of the most ICONIC and NATURAL things mandated by Evolution, Treat your Body to the Health-giving Benefits of SLEEP, DIET and EXERCISE!

We tested the hypothesis that apathy, but not depression, is associated with dementia in patients with SVD. We found that higher baseline apathy, as well as increasing apathy over time, were associated with an increased dementia risk. In contrast, neither baseline depression or change in depression was associated with dementia. The relationship between apathy and dementia remained after controlling for other well-established risk factors including age, education and cognition. Finally, adding apathy to models predicting dementia improved model fit. These results suggest that apathy may be a prodromal symptom of dementia in patients with SVD.
Cerebral small vessel disease (SVD) is the leading vascular cause of dementia and plays a major role in cognitive decline and mortality.1 2 SVD affects the small vessels of the brain, leading to damage in the subcortical grey and white matter.1 The resulting clinical presentation includes cognitive and neuropsychiatric symptoms.1
Apathy is a reduction in goal-directed behaviour, which is a common neuropsychiatric symptom in SVD.3 Importantly, apathy is dissociable from depression,3 4 another symptom in SVD for which low mood is a predominant manifestation.5 Although there is some symptomatic overlap between the two,6 research using diffusion imaging reported that apathy, but not depression, was associated with white matter network damage in SVD.3 Many of the white matter pathways underlying apathy overlap with those related to cognitive impairment, and accordingly apathy, rather than depression, has been associated with cognitive deficits in SVD.7 These results suggest that apathy and cognitive impairment are symptomatic of prodromal dementia in SVD.
From a Wall Street Journal article (May 21, 2020):
Breathing properly can allow us to live longer and healthier lives. Breathing poorly, by contrast, can exacerbate and sometimes cause a laundry list of chronic diseases: asthma, anxiety, attention deficit hyperactivity disorder, hypertension and more. Poor breathing habits can even change the physical structure of our skeletons, depleting essential minerals and weakening our bones.

Most of us misunderstand breathing. We see it as passive, something that we just do. Breathe, live; stop breathing, die. But breathing is not that simple and binary. How we breathe matters, too.
Last year, I wanted to see just how dramatically breathing habits—good and bad ones—could affect my own brain and body. I’d learned that up to 50% of us are chronic mouth breathers, a problem well described by an ancient Tao text: “The breath inhaled through the mouth is called ‘Ni Ch’i, adverse breath,’ which is extremely harmful.”
Scientists have known for decades that inhaling through this pathway saps the body of moisture, irritates the lungs and loosens the soft tissues at the back of the mouth. Mouth breathing has also been linked with neurological disorders, periodontal disease and increased risk of respiratory infection. But nobody knew how quickly this damage came on.
COMMENTARY
Breathing is something we don’t think about. It comfortably transcends the merely habitual, and there is a complex of controllers in the brain to Drive breathing should we be unable or forget to breathe voluntarily.
Breathing has it’s own poets and cults, one of which is MINDFULNESS MEDITATION, which uses our BREATHING as the focus of our consciousness, to get us outside ourselves.
With DEEP breathing, I noticed an INCREASED pO2, as registered on my Pulse Oximeter.
In the 1960’s asthma was not so well controlled as now. The mechanics of breathing were more important, so we taught our Patients how to breathe properly.
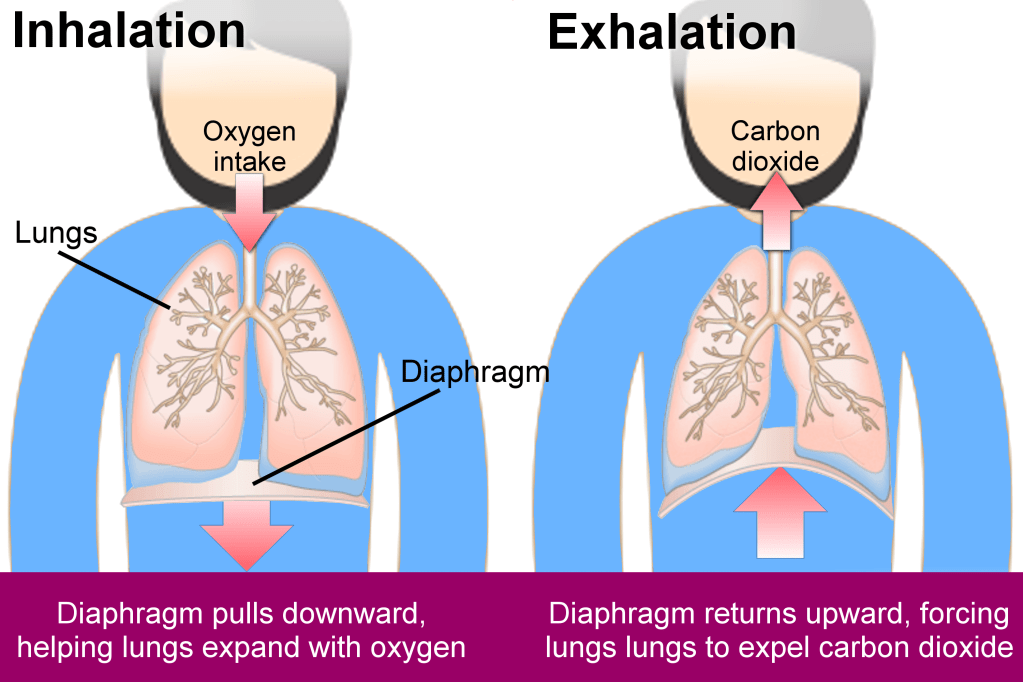
There are 2 sets of muscles we use to EXPAND our lungs, the DIAPHRAGM at the bottom of the chest, and the chest muscles themselves, the INTERCOSTALS. We refer to diaphragmatic breathing as “stomach” breathing, because the stomach bulges out as the descending diaphragm compresses the abdominal contents.
We refer to intercostal breathing as “chest” breathing because the chest expands when the inspiratory intercostals contract.
Diaphragmatic breathing is more efficient, and we encourage our asthmatic patients to Use their more efficient diaphragm to prevent them from tiring as they struggle to get their air out through their narrated airways.
You can squeeze a little extra air out of your lungs by contracting your abdominal muscles.
So to take a DEEP BREATH, see that your stomach rises and your chest expands with the breath IN, and that you squeeze both your abdomen and your chest with the breath out.
Your AIR SACS expand, your lungs are flushed with fresh air, and you blood oxygen, and BRAIN OXYGEN INCREASES with a deep breath in. The “stale air” is cleared by a full breath out.
When you are quietly breathing, letting that vital process take place automatically, notice that a deep breath, or “sigh”, occurs about once every 2 minutes. This is nature’s way to help lung surfactant PREVENT LUNG COLLAPSE and PNEUMONIA.
It is HEALTHFUL to PAY ATTENTION to your BREATHING occasionally! If uninclined to breathe deeply yourself, take a brisk walk up a hill, and let Nature do it for you.