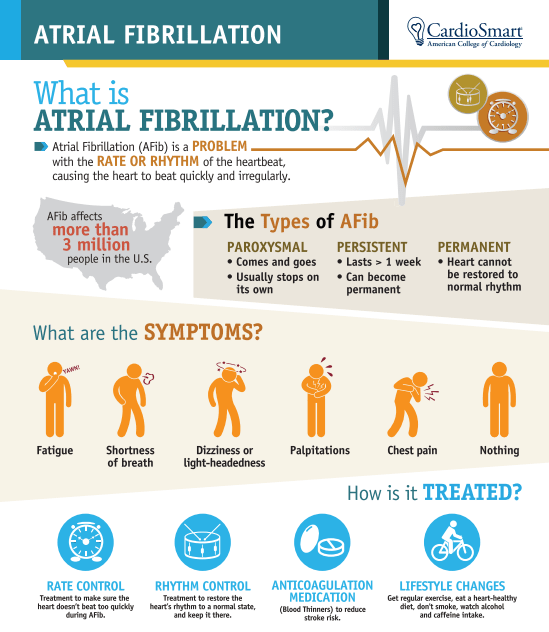
In this instructional video, Drs. Jane Leopold, Elliott Antman, William Sauer, and Paul Zei provide an overview of the classification and diagnosis of atrial fibrillation, management strategies, and mitigation of stroke risk with anticoagulation therapy.
Video timeline: 0:00 Pathophysiology and Symptoms 3:11 Stroke Risk, Anticoagulants, and Arrhythmia Control 6:32 Catheter Ablation 10:11 Post-Procedural Monitoring and Care
The video also focuses on the new rhythm-control strategy of catheter ablation therapy, with attention to the success rate, potential complications, postprocedural monitoring for recurrence of atrial fibrillation, and consideration of ongoing anticoagulation therapy in these patients. The New England Journal of Medicine is the world’s leading general medical journal.
Continuously published for over 200 years, the Journal publishes peer-reviewed research along with interactive clinical content for physicians, educators, and the global medical community at https://NEJM.org.
COMMENTARY:
This is a very good video well worth watching by general physicians and interested patients. There are several general and some specific comments I would like to make.
First, in my opinion, the best physician is none too good. In any operative or serious procedure, the decision to operate should be made by the patient in conjunction with a physician that does not do the operating. In my case, as a physician, I consulted an electrophysiologist.
Second, in my opinion, a good medicine is better than surgery. For atrial fibrillation, there has been no new medication treatment for decades. The main drugs are still amiodarone and Propafenone. The latter is less consistently effective, but has a better long-term safety profile; amiodarone often produces ‘floaters” in the eye, and Propafenone merely a bitter taste which you’ll get used to.
Third, it must be realized that catheter ablation is often not curative, especially as you get older, which was rather glossed over in this video. Ablation also requires a great deal of expensive equipment, which is constantly evolving, hence the importance of getting your ablation at a major center where it is done all the time. These major centers have less complications such as atrial wall perforation; Yes, you can rarely wind up worse off after any operation.
I am a physician, currently 90 years old. I developed atrial fibrillation of the persistent type when I was in my late 70s. I had a cardioversion to get me into sinus rhythm, and then tried Propafenone, which kept me in sinus rhythm for less than a month. My main motivation to get a radio frequency ablation was to stay off of anticoagulants. I had my ablation, and remained in sinus rhythm, and off anticoagulants, for three years. I could always tell when I went into atrial fibrillation from normal sinus rhythm because I produced a lot of urine and had to go to the bathroom all the time; atrial fibrillation causes release of a hormone called atrial naturetic peptide. I could also tell by taking my own pulse, which was quite irregular in comparison to my very regular sinus rhythm pulse, which ticked along with a rate in the high 50s. I had always thought my rate was low because I exercise a lot. Actually, my EKG shows a second-degree heart block which is probably partially responsible.
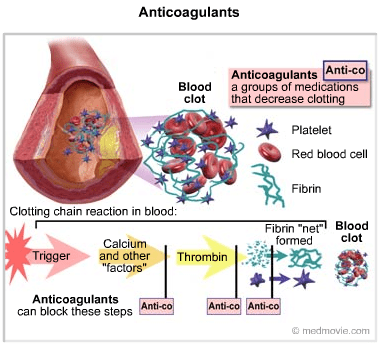
After three years, I returned to atrial fibrillation, and needed a another ablation. They found very few areas of abnormal electrical activity, and gave me a “touchup”, which lasted another two or three years after which I went back into atrial fibrillation. Probably as a result of my age, a fibrillated at a slow rate, and at least did not need any extra medication for rate control, although I did, of course, need to take a regular anticoagulant, in my case Eliquis.
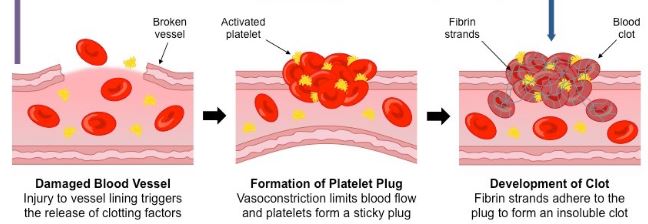
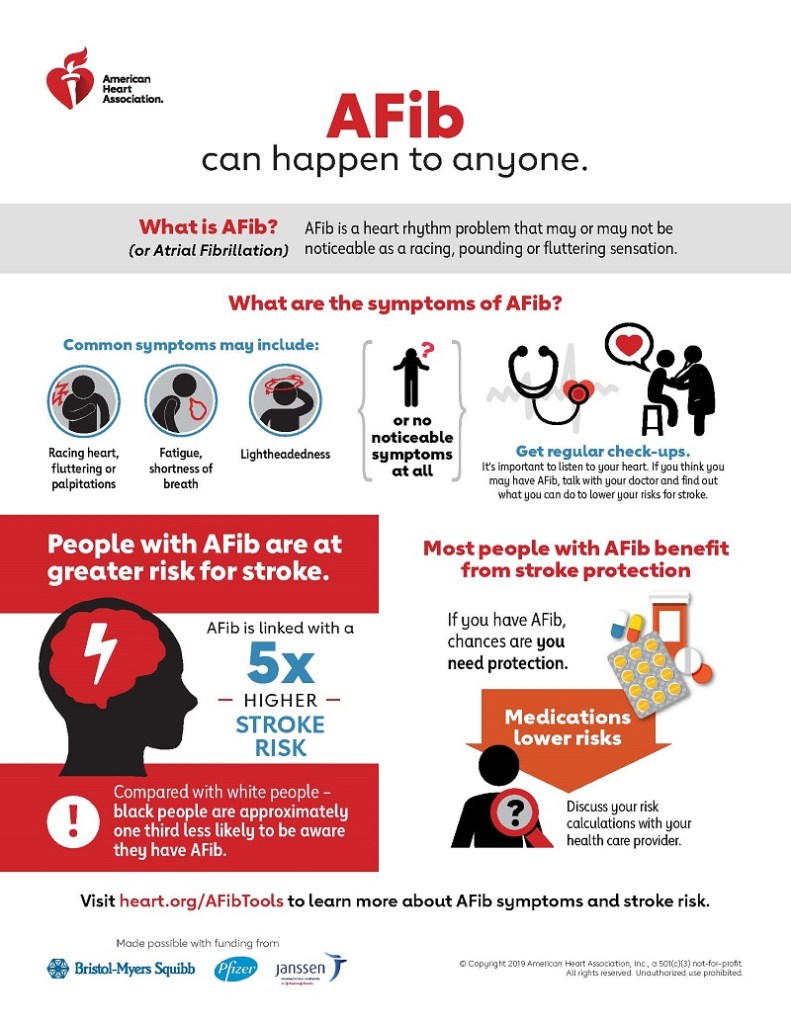
In summary, atrial fibrillation is a common electrical storm in the upper chambers of the heart, causing a rapid, irregular beat. AF increases in frequency as you get older. In the video they mention the “substrate”, which is the structure of the atrium. In my own case, this was an enlarged atrium, and probably a tendency towards atrial fibrillation; my brother also has AF. The main complication is stagnation of blood in the atria, resulting in increased tendency toward stroke. Fibrillation therefore requires an anticoagulant.
There is some discussion about the irregular rate causing an inefficiency of cardiac action, contributing to heart failure, This is logical, but not clear cut statistically.
—Dr. C.