Crohn’s disease is an inflammatory bowel disease that is characterized by chronic inflammation of any part of the gastrointestinal tract, has a progressive and destructive course and is increasing in incidence worldwide. Several factors have been implicated in the cause of Crohn’s disease, including a dysregulated immune system, an altered microbiota, genetic susceptibility and environmental factors, but the cause of the disease remains unknown. The onset of the disease at a young age in most cases necessitates prompt but long-term treatment to prevent disease flares and disease progression with intestinal complications. Thus, earlier, more aggressive treatment with biologic therapies or novel small molecules could profoundly change the natural history of the disease and decrease complications and the need for hospitalization and surgery. Although less invasive biomarkers are in development, diagnosis still relies on endoscopy and histological assessment of biopsy specimens. Crohn’s disease is a complex disease, and treatment should be personalized to address the underlying pathogenetic mechanism. In the future, disease management might rely on severity scores that incorporate prognostic factors, bowel damage assessment and non-invasive close monitoring of disease activity to reduce the severity of complications.
Tag Archives: Chronic Inflammation
Health: Four Tests For Chronic Inflammation
These are four of the most common tests for inflammation:
- Erythrocyte sedimentation rate (sed rate or ESR). This test measures how fast red blood cells settle to the bottom of a vertical tube of blood. When inflammation is present the red blood cells fall faster, as higher amounts of proteins in the blood make those cells clump together. While ranges vary by lab, a normal result is typically 20 mm/hr or less, while a value over 100 mm/hr is quite high.
- C-reactive protein (CRP). This protein made in the liver tends to rise when inflammation is present. A normal value is less than 3 mg/L. A value over 3 mg/L is often used to identify an increased risk of cardiovascular disease, but bodywide inflammation can make CRP rise to 100 mg/L or more.
- Ferritin. This is a blood protein that reflects the amount of iron stored in the body. It’s most often ordered to evaluate whether an anemic person is iron-deficient, in which case ferritin levels are low. Or, if there is too much iron in the body, ferritin levels may be high. But ferritin levels also rise when inflammation is present. Normal results vary by lab and tend to be a bit higher in men, but a typical normal range is 20 to 200 mcg/L.
- Fibrinogen. While this protein is most commonly measured to evaluate the status of the blood clotting system, its levels tend to rise when inflammation is present. A normal fibrinogen level is 200 to 400 mg/dL.
Commentary:
Inflammation is an essential, evolutionarily conserved mechanism that our bodies have developed for excluding infections, toxins, and damaged or cancerous cells.
Acute inflammation in response to infections is almost always beneficial, except where it is disproportionate to the danger that it fights; the common cold is probably innocuous, but we develop symptoms from our bodies’ response. Covid has been found to incite disproportionately severe inflammation, which can lead to severe disease, and the need for corticosteroids.
Chronic inflammation is a different animal, and is usually undesirable. Sometimes it is due to an infection, such as tuberculosis, which won’t go away. Sometimes the bodies immune system develops a disordered communication system, and fights its own cells, called auto immunity.
Chronic inflammation can also be caused by obesity, chronic stress, cigarette smoking, alcohol in excess, and cancer, which can also be CAUSED BY chronic inflammation.
Chronic inflammation is also associated with Alzheimer’s, heart disease, rheumatoid arthritis, and type two diabetes. Asthma is a chronic inflammatory disease of the airways. IBD, inflammatory bowel disease, is a chronic inflammatory disease of the intestinal tract.
The symptoms of chronic inflammation very widely depending on the area involved. Abdominal pain, chest pain, joint pain, skin rashes, fatigue, and fever are some of the symptoms.
You can reduce your likelihood of chronic inflammation by maintaining normal weight, having regular exercise, eating a diet rich in natural vegetables and fruits (antioxidants), avoiding alcohol and cigarette smoke, and by reducing or handling your stress.
—Dr. C.
Inflammation: Three Ways It Affects Your Health
Acute inflammation happens as a part of our defense mechanism to clear out pathogens. So when a virus or bacteria invades us, we need to quickly mount an acute inflammatory response to get rid of the pathogen. Sometimes, that acute immune response isn’t enough to get rid of the pathogen. That’s when we elevate the level to the adaptive immune response. That’s when you involve specific lymphocytes, T and B cells, to fight off the infection.
So inflammation is a necessary process for dealing with pathogens but sometimes, it can also turn against us. Chronic inflammation happens because the body fails to get rid of the cause of the inflammation, such as viruses and bacteria. In those conditions, such as, you know, chronic infection with HIV or hepatitis virus or lung COVID, in which case we there may be a persistent viral reservoir that’s causing this chronic inflammation, the inflammation itself becomes the enemy.
Even though inflammation evolve to counter pathogens, it’s also engaged by other causes, and so having this amount of fat, for example, alone is able to trigger the immune system and induce the chronic inflammatory response that then fuels further problems to happen because the body is sort of trying to fight off a non-existent infection and therefore, it can sort of engage a chronic state of inflammation.
I can’t think of a disease which doesn’t involve inflammation, but we are now learning more and more about the physiological role of inflammation. Homeostasis ensures that we have a normal operation of different physiological functions like heart rate, breathing and glucose levels or insulin levels. Those two system, the inflammatory system and the homeostasis, they work together to maintain each other. Sometimes, the inflammatory response has to override the homeostatic response.
That includes things like adaptation to a different diet. The immune cells are now known to be able to sense differences in dietary conditions and adapt the intestine for future absorption of nutrients. This kind of events that are not necessarily at all related to pathogens, but for maintaining physiology. Inflammatory responses are integral in order to maintain health. So a molecular-level understanding of inflammation is necessary to understand the logic by which these systems function, and also it provides the pharmaceutical target for future therapies of inflammatory diseases.
THE DOCTORS 101 CHRONIC SYMPTOMS & CONDITIONS #52: RHEUMATOID ARTHRITIS
Painful, stiff joints are almost the rule as we get older, it seems. Both osteoarthritis and rheumatoid arthritis contribute to that eventuality. Osteoarthritis typically worsens as we get older, whereas rheumatoid arthritis starts in middle age.
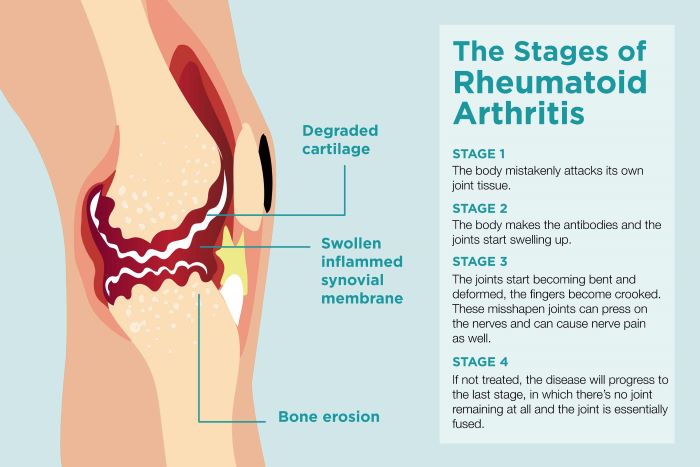
Rheumatoid arthritis is much more severe than osteoarthritis, since it is an autoimmune condition with an episodic inflammatory component. A recent medical study of different blood substances found that the “metabolome” has many markers for exacerbation of rheumatoid arthritis.
The main test currently being used to show exacerbation is CRP, C-reactive protein. Rheumatoid factor tests, such as anti-CCP, are used to confirm the diagnosis.
Rheumatoid arthritis tends to involve the small joints of the hand, and osteoarthritis the larger joints, such as the hips and knees. I go a bit against the grain, having diagnosed osteoarthritis of my fingers and toes, more typical of RA, but, even at the age of 89, my large joints are still in good shape, even with a lot of walking. Since walking is thought to increase the perfusion of joint fluid to nourish the knee cartilages, perhaps I should say BECAUSE of walking. Running tends to wear the knees and hips out, because of high impact on the joints.
The inflammation of rheumatoid arthritis tends to wax and wane, but during an exacerbation can be quite incapacitating. The interleukin TNF seems instrumental in causing these flares, and antibodies directed towards TNF, such as etanercept, has been a helpful treatment. This injection is also given for other inflammatory, autoimmune conditions such as psoriasis, particularly psoriatic arthritis, and the inflammatory bowel diseases.
Almost half the people who have rheumatoid arthritis also experience signs and symptoms in other tissues, such as the skin, eyes, heart, and lungs. It is truly a systemic, autoimmune disease.
For more information please consult the following mayo clinic article on rheumatoid arthritis.