
INFOGRAPHIC: ‘BENEFITS OF PROBIOTICS’ ON EXERCISE PERFORMANCE & HEALTH


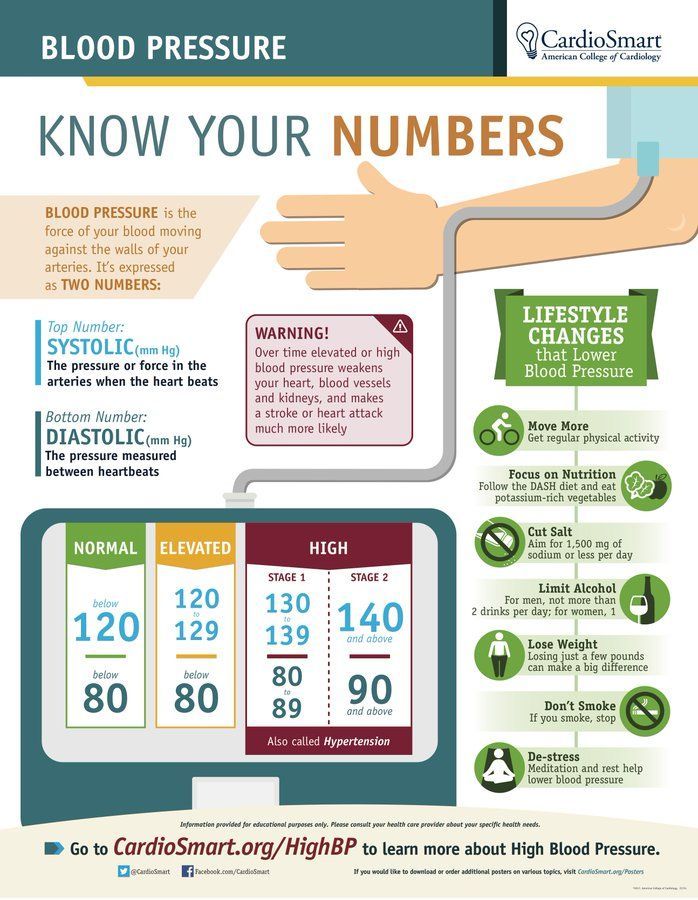
Hypertension places an extra load on the blood vessels and heart, and eventually causes them to become diseased. High Blood Pressure is therefore bad for the entire body, which depends on the blood vessels for delivering the nutrients and oxygen necessary for life.
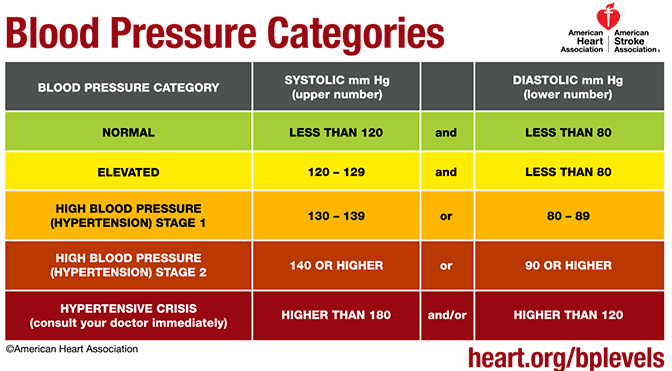
Most hypertension happens from subtle changes in the body’s signalling systems, and often runs in families; This is called “essential hypertension”. Additionally, there are a number of diseases and conditions of which hypertension is a symptom. It is important to know if you have hypertension, and fortunately it is easy to discover.
A visit to the doctor, or even to the pharmacy will make a reading available, and if you are concerned, an automatic cuff is available for $20. A healthy lifestyle and weight Will help prevent and treat hypertension, as in so many other chronic conditions.
A variety of medications are available to treat hypertension, but ANY MEDICATION CAN PRODUCE SIDE EFFECTS. It is rare for an effective medication to produce only a single, desired effect on the body. I have never known a person who at some time did not experience some side effect from antihypertensive medications.
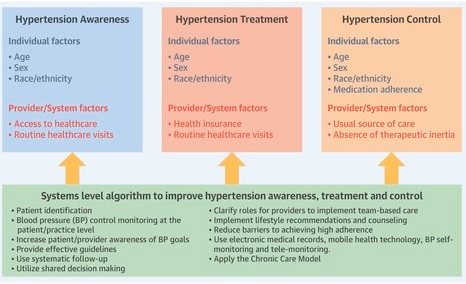
Be sure to maintain contact with your Doctor. The dose may be too high, causing episodes of LOW blood pressure with fainting. When I was in practice, any number of patients came to me with a chronic cough, which I “cured” by having their doctor replace their ACE Inhibitor with another medication.
Please read the accompanying Mayo Clinic article for a complete discussion of this important condition.
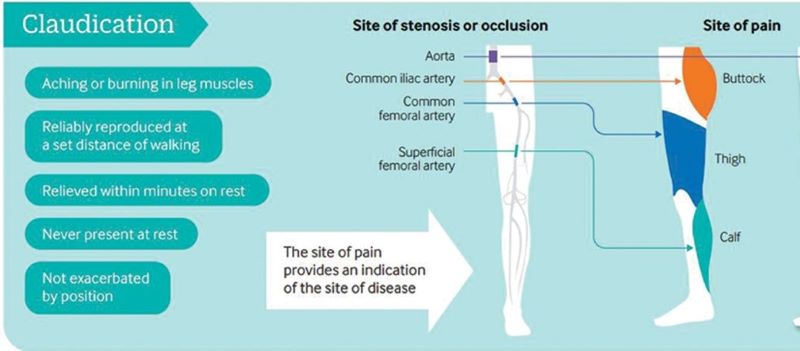
Exercise training is a safe, effective and low-cost intervention for improving walking ability in patients with IC. Additional benefits may include improvements in QoL, muscle strength and cardiorespiratory fitness. Clinical guidelines advocate supervised exercise training as a primary therapy for IC, with walking as the primary modality.
However, evidence is emerging for the role of various other modes of exercise including cycling and progressive resistance training to supplement walking training. In addition, there is emerging evidence for home-based exercise programmes. Revascularisation or drug treatment options should only be considered in patients if exercise training provides insufficient symptomatic relief.
Peripheral artery disease (PAD) is caused by atherosclerotic narrowing of the arteries supplying the lower limbs often resulting in intermittent claudication, evident as pain or cramping while walking. Supervised exercise training elicits clinically meaningful benefits in walking ability and quality of life. Walking is the modality of exercise with the strongest evidence and is recommended in several national and international guidelines. Alternate forms of exercise such as upper- or lower-body cycling may be used, if required by certain patients, although there is less evidence for these types of programmes. The evidence for progressive resistance training is growing and patients can also engage in strength-based training alongside a walking programme. For those unable to attend a supervised class (strongest evidence), home-based or ‘self-facilitated’ exercise programmes are known to improve walking distance when compared to simple advice. All exercise programmes, independent of the mode of delivery, should be progressive and individually prescribed where possible, considering disease severity, comorbidities and initial exercise capacity. All patients should aim to accumulate at least 30 min of aerobic activity, at least three times a week, for at least 3 months, ideally in the form of walking exercise to near-maximal claudication pain.
Health experts say having a vaccine is just one front in a two-front battle against COVID-19. The other is effective treatments for those who are already sick with the disease. WSJ breaks down the three most promising types in development. Photo Illustration: Jacob Reynolds/WSJ.

The number of older people, including those living with dementia, is rising, as younger age mortality declines. However, the age-specific incidence of dementia has fallen in many countries, probably because of improvements in education, nutrition, health care, and lifestyle changes.
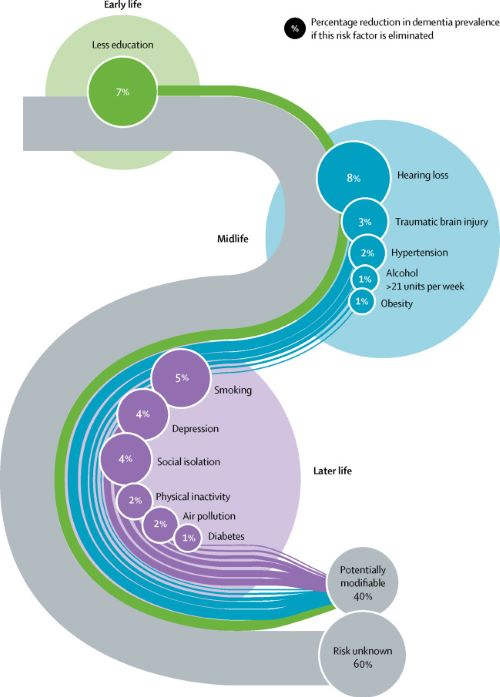
Overall, a growing body of evidence supports the nine potentially modifiable risk factors for dementia modelled by the 2017 Lancet Commission on dementia prevention, intervention, and care: less education, hypertension, hearing impairment, smoking, obesity, depression, physical inactivity, diabetes, and low social contact.
We now add three more risk factors for dementia with newer, convincing evidence. These factors are excessive alcohol consumption, traumatic brain injury, and air pollution. We have completed new reviews and meta-analyses and incorporated these into an updated 12 risk factor life-course model of dementia prevention. Together the 12 modifiable risk factors account for around 40% of worldwide dementias, which consequently could theoretically be prevented or delayed.
The potential for prevention is high and might be higher in low-income and middle-income countries (LMIC) where more dementias occur. Our new life-course model and evidence synthesis has paramount worldwide policy implications. It is never too early and never too late in the life course for dementia prevention. Early-life (younger than 45 years) risks, such as less education, affect cognitive reserve; midlife (45–65 years), and later-life (older than 65 years) risk factors influence reserve and triggering of neuropathological developments.
Culture, poverty, and inequality are key drivers of the need for change. Individuals who are most deprived need these changes the most and will derive the highest benefit.
Read full Dementia Study and Report
COMMENTARY:
Lancet’s 2017 Metanalysis mentions 9 Dementia risk factors. The 2020 Paper adds 3 additional factors. TRAUMATIC BRAIN INJURY, ALCOHOLISM, and AIR POLLUTION.
The inclusion of Trauma, with a 3% weighting, may be due to the increased awareness of TBE stemming from football injuries. The preventable 12 Factors are still in the minority. 60% of the factors are not preventable, since they are Genetically determined.
LESS EDUCATION, HEARING LOSS and SOCIAL ISOLATION, 3 of the original 9 factors,all lead to less brain stimulation, and can be unified under the idea of COGNITIVE RESERVE. If a person starts with less Cognition, it is reasonable to think he would be Demented sooner.
Together, less education, hearing loss, and social isolation account for almost Half of the correctable conditions. SMOKING is one of those things which impact almost every human disorder. It is amazing that cigarettes are still manufactured. In fact, their use is actually Increasing,especially the Far East, where they probably account for much of the escalating problem with Dementia in that region.
Our favorite causes, Sleep, Diet, and Exercise, apparently play only a minor role in Dementia. Sleep is completely dismissed in this report. The fact that both Sleeping less than the Ideal 7-8 hours, and more than that amount is thought to correlate with health problems is probably the main reason for the omission.
My own opinion is that people who are in poor health may need more sleep, and therefore sleep longer. My own sleep is interrupted 3-5 times per night, so it is not surprising that I need an hour extra to feel rested. Any less than 9-10 hours, and I need a nap, which in my opinion is a sign of insufficient nighttime sleep. Poor sleep may be a factor in metabolic syndrome, often leading to DIABETES, OBESITY, and HYPERTENSION, which are factors in Dementia, mentioned in the article as bit players.
PHYSICAL INACTIVITY is mentioned as a minor factor in Dementia, but exercise, studied as a treatment of dementia, was found to improve only strength. Diet is not mentioned, but does contribute to OBESITY, which is a minor factor. Dementia is a great emotional and economic burden, afflicting many otherwise happy families with misfortune.
The Lancet metanalysis is admirable. But don’t forget the healthy lifestyle emphasizing Sleep Diet and Exercise; and exercise includes cognitive exercise. Anything we can do to avoid dementia is worthwhile. –
Anthony S. Fauci, MD returns to JAMA’s Q&A series to discuss the latest developments in the COVID-19 pandemic, including the continued importance of nonpharmaceutical interventions (masking, handwashing, physical distancing) for managing rising case numbers in the US and globally.
Recorded October 28, 2020.
Topics discussed in this interview: 0:00 Introduction 0:20 NAM Presidential Citation for Exemplary Leadership 1:19 COVID-19 numbers and excess deaths 4:05 National masking mandate 5:55 How to get people to accept masking 7:07 Herd Immunity and the Great Barrington Declaration 9:51 The holidays and airplane travel 13:44 Therapies update 17:54 Vaccines update 20:08 Vaccine distribution 22:00 Vaccine safety 24:42 How Australia has dealt with COVID-19 spikes 27:00 Acknowledgements and baseball

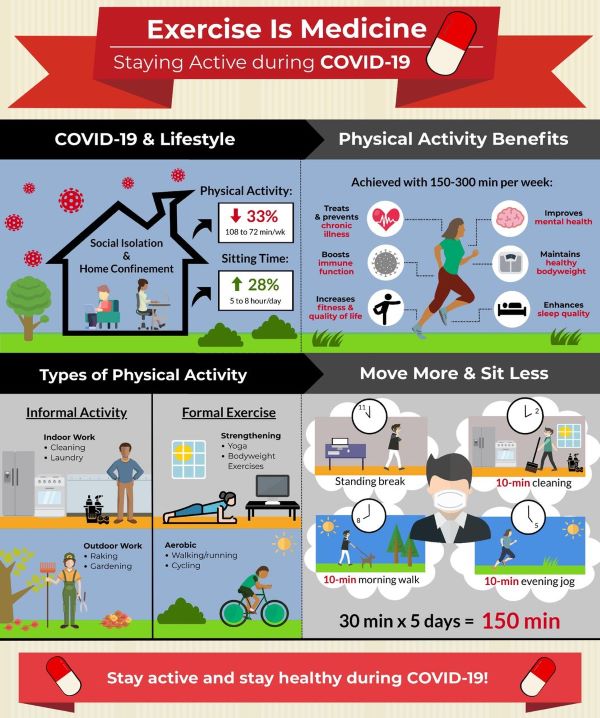

There are over 35,000,000 reported cases of COVID-19 disease and 1 000 000 deaths across more than 200 countries worldwide.1 With cases continuing to rise and a robust vaccine not yet available for safe and widespread delivery, lifestyle adaptations will be needed for the foreseeable future. As we try to contain the spread of the virus, adults are spending more time at home. Recent evidence2 suggests that physical activity levels have decreased by ~30% and sitting time has increased by ~30%. This is a major concern as physical inactivity and sedentary behaviour are risk factors3 for cardiovascular disease, obesity, cancer, diabetes, hypertension, bone and joint disease, depression and premature death.
To date, more than 130 authors from across the world have provided COVID-19-related commentary on these concerns. Many experts4 have emphasised the importance of increasing healthy living behaviours and others5 have indicated that we are now simultaneously fighting not one but two pandemics (ie, COVID-19, physical inactivity). Physical inactivity alone results in over 3 million deaths per year5 and a global burden of US$50 billion.6 Immediate action is required to facilitate physical activity during the COVID-19 pandemic because it is an effective form of medicine3 to promote good health, prevent disease and bolster immune function. Accordingly, widespread messaging to keep adults physically active is of paramount importance.
Several organisations including the WHO, American Heart Association and American College of Sports Medicine have offered initial suggestions and resources for engaging in physical activity during the COVID-19 pandemic. Expanding on these resources, our infographic aims to present a comprehensive illustration for promoting daily physical activity to the lay audience during the COVID-19 pandemic (figure 1). As illustrated, adults are spending more time at home, moving less and sitting more. Physical activity provides numerous health benefits, some of which may even help directly combat the effects of COVID-19. For substantial health benefits, adults should engage in 150–300 min of moderate-to-vigorous intensity physical activity each week and limit the time spent sitting. The recommended levels of physical activity are safely attainable even at home. Using a combination of both formal and informal activities, 150 min can be reached during the week with frequent sessions of physical activity spread throughout the day. Sedentary behaviour can be further reduced by breaking up prolonged sitting with short active breaks. In summary, this infographic offers as an evidence-based tool for public health officials, clinicians, educators and policymakers to communicate the importance of engaging in physical activity during the COVID-19 pandemic.
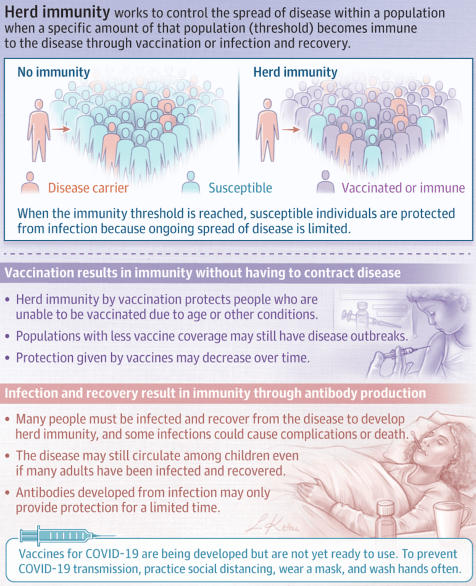
Herd immunity occurs when a significant portion of a population becomes immune to an infectious disease, limiting further disease spread.
Disease spread occurs when some proportion of a population is susceptible to the disease. Herd immunity occurs when a significant portion of a population becomes immune to an infectious disease and the risk of spread from person to person decreases; those who are not immune are indirectly protected because ongoing disease spread is very small.
The proportion of a population who must be immune to achieve herd immunity varies by disease. For example, a disease that is very contagious, such as measles, requires more than 95% of the population to be immune to stop sustained disease transmission and achieve herd immunity.
Herd immunity may be achieved either through infection and recovery or by vaccination. Vaccination creates immunity without having to contract a disease. Herd immunity also protects those who are unable to be vaccinated, such as newborns and immunocompromised people, because the disease spread within the population is very limited. Communities with lower vaccine coverage may have outbreaks of vaccine-preventable diseases because the proportion of people who are vaccinated is below the necessary herd immunity threshold. In addition, the protection offered by vaccines may wane over time, requiring repeat vaccination.
Achieving herd immunity through infection relies on enough people being infected with the disease and recovering from it, during which they develop antibodies against future infection. In some situations, even if a large proportion of adults have developed immunity after prior infection, the disease may still circulate among children. In addition, antibodies from a prior infection may only provide protection for a limited duration.
People who do not have immunity to a disease may still contract an infectious disease and have severe consequences of that disease even when herd immunity is very high. Herd immunity reduces the risk of getting a disease but does not prevent it for nonimmune people.
There is no effective vaccine against coronavirus disease 2019 (COVID-19) yet, although several are currently in development. It is not yet known if having this disease confers immunity to future infection, and if so, for how long. A large proportion of people would likely need to be infected and recover to achieve herd immunity; however, this situation could overwhelm the health care system and lead to many deaths and complications. To prevent disease transmission, keep distance between yourself and others, wash your hands often with soap and water or sanitizer that contains at least 60% alcohol, and wear a face covering in public spaces where it is difficult to avoid close contact with others.