#Gallbladder polyps: Can they be cancerous? Dr. Sahil Khanna, a @MayoClinic gastroenterologist, explains. #GallbladderCancer https://t.co/oXqGpUynOb pic.twitter.com/NnYH0K2WqE
— Mayo Clinic Comprehensive Cancer Center (@MayoCancerCare) January 8, 2022
Monthly Archives: January 2022
Nervous System: Multiple Sclerosis Explained (Mayo)
Learning about multiple sclerosis can be intimidating. Let our experts walk you through the facts, the questions, and the answers to help you better understand this condition.
Video timeline: 0:24 What is multiple sclerosis? 1:15 Types of multiple sclerosis 1:29 Who gets multiple sclerosis/risk factors? 3:11 Multiple sclerosis symptoms 3:40 How is multiple sclerosis diagnosed? 4:39 Treatment options 5:29 Coping methods/ What now? 6:23 Ending
For more reading visit: https://mayocl.in/3t24QSG
Back Pain: The Symptoms And Causes Of Sciatica
Most sciatica is caused by problems that affect the L4, L5, or S1 nerve roots. The nerve may be compressed or irritated, usually because it’s being rubbed by a disc, bone, joint, or ligament. The resulting inflammation makes the tissues and the nerves more sensitive and the pain feel worse.
Damage to or pinching of the sciatic nerve, or the nerves that feed into it, can have several causes.
Herniated disc
One of the most common causes of sciatica is a herniated disc in the lower part of the spine. It’s also called a slipped disc, though there’s no slipping going on.
Spinal discs are tucked between the vertebrae, where they act as cushions to keep the bones from touching one another. The discs absorb all the forces placed on the spine from walking, running, sitting, twisting, lifting, and every other activity we do. They also absorb forces from falls, collisions, and other accidents.
Spinal stenosis
The spinal canal protects the spinal cord and the nerves that run up and down the spine. Spinal stenosis is the narrowing of the spinal canal. When this occurs, nerves can be compressed, causing pain. Because the lumbar vertebrae undergo the most consistent stress and support the most weight, lumbar stenosis is the most common type of spinal stenosis.
Spondylolisthesis
The bones of the spine are stacked on top of one another, separated by discs. Spondylolisthesis occurs when one spinal bone slips forward in relation to the bone below it. When the L4 vertebra moves over the L5 vertebra, it can cause a kink in the spinal canal leading to pressure on a nerve root and sciatica.
Read more
Dr. C’s Journal: Pain Without Treatable Cause
Pain is useful to survival, and therefore is evolutionarily conserved. There is a very rare syndrome with the congenital inability to experience pain that Is caused by mutations in the SCN9A gene, which codes for a sodium channel (Nav 1.7). Research on this channel has apparently produced some advances in pain medication, but not as much as expected.
Individuals with insensitivity to pain have many accidental injuries which can cause blindness, mutilations of the extremities, and other severe problems. Lack of ability to feel pain is serious handicap.
Pain is generally a useful red flag that warns us to stop the painful activity, or guides us into the doctors office; about half of all medical visits involve pain of some sort.
Considered as a symptom, pain helps guide the physician into the proper diagnosis and treatment. Normally the pain stops when the condition that produced it is corrected. Pain sometimes outlives it’s usefulness, however, and becomes a major problem on his own. The most obvious condition is “phantom limb pain”. Most people who have had an amputation will continue to experience pain in the extremity that is no longer present.
Back pain that has no valid surgical treatment will sometimes drive individuals to surgeons who will operate on them unsuccessfully. A second opinion, preferably by a medical doctor like a neurologist, is always a good idea with back pain without sciatica, numbness, or other localizing symptom to tell the doctor where to operate.
Neuropathic pain is another conundrum. I know of an individual who was bitten on the foot by a dog, and continued to have severe foot pain for many years after the original injury healed.
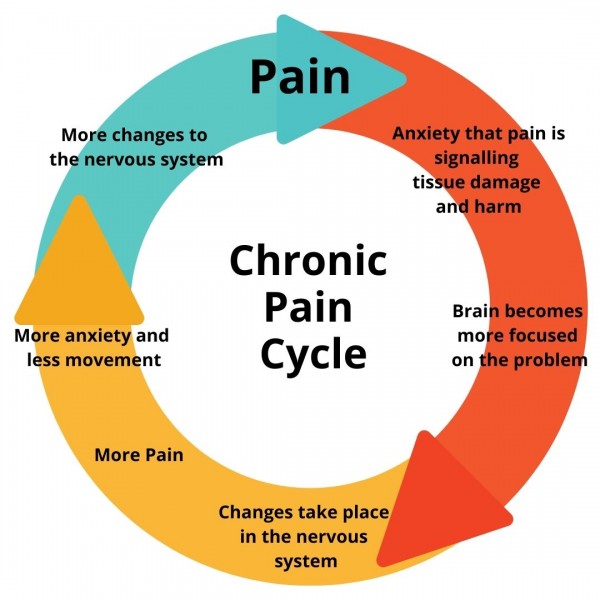
All pain is interpreted in the brain, and continuing circles of central nerve activation is the leading theory of phantom limb and neuropathic pain. Pain is not objectively measurable; there is no meter that you can attach to the patient and find how much pain they are actually having. The doctor must assume that the patient has the pain they are describing, and ask the patient to rate it on a 0 to 10 scale, describe its severity, time course, quality, and any factors that will make it better or worse. Most often this produces an avenue to treatment, but sometimes not.
A few decades ago, busy doctors would label the pain that they could not diagnose as “psychological”, and dismiss the patient to suffer in silence. Much of the pain, however, was very real to the patients, who joined in patient advocacy groups and produced a political backlash which induced doctors to overtreat the pain, often with opioids.
The over-prescribing doctors, and unscrupulous drug companies led to the flooding of the market with opioid medication, leading to the opioid crisis that is now being addressed. There is difficulty in making scientific progress on an adversary that cannot be measured properly.
Some doctors, usually anesthesiologists, specialize in treating the chronic, severe pain that standard medical practice has been unable to diagnose or alleviate.
They may use nerve blocks, antidepressants and combinations of different pain medication. Judicious propofol has been used also not only for chronic undiagnosed pain, but also depression.
My wife had a pain problem which responded to a combination of two simple medications, motrin and acetaminophen. The suggested overall approach is to get the best medical care available to diagnose the cause of the pain, and ask for a pain management referral if a solution is not found.
More information can be found in the appended Wikipedia article.
—Dr. C.
DOCTORS PODCAST: MEDICAL & TELEHEALTH NEWS (JAN 3)
A weekly podcast on the latest medical, science and telehealth news.







