A thoracic aortic aneurysm is a weak spot in the aorta, the main pipeline for blood from the heart to the body. The weak spot has the potential to dissect or rupture, cutting off the supply of life-sustaining blood to the rest of the body. Thoracic aortic aneurysms are often harder to detect and diagnose compared to the more common abdominal aortic aneurysms.

The aorta begins deep in the heart. It emerges from the top of the powerful left ventricle, curves up and over the heart in a gentle arch, then descends into the chest and through the muscular diaphragm into the abdomen (see “Thoracic aorta”). It ends around the belly button, where it splits into two smaller arteries, one for each leg.
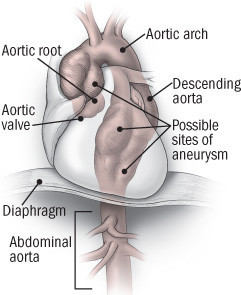
From start to end, arteries branch off to nourish the heart, brain, arms, kidneys, liver, stomach, intestines, and every other part of the body. The stretch of the aorta from its start in the heart to the top of the diaphragm is called the thoracic aorta; the section below the diaphragm is the abdominal aorta.
Some aneurysms are relatively harmless. Others can lead to the catastrophic problems known as dissection or rupture. For now, size is the best and only guide to the health threat posed by an aneurysm.
Dissection. The most common consequence of an aortic aneurysm, dissection occurs when a tear develops in the inner lining of the aortic wall. The inner and outer layers peel apart, creating an extra channel for blood inside the aorta. It may do no harm, or it may allow blood to bypass the outflow to certain organs or tissues, leaving them without a blood supply. This can cause a heart attack, stroke, kidney damage, and other problems.
Rupture. A break in all three layers of the aortic wall is termed a rupture. Blood pours from the aorta into the chest. This massive internal bleeding can quickly lead to shock and death.