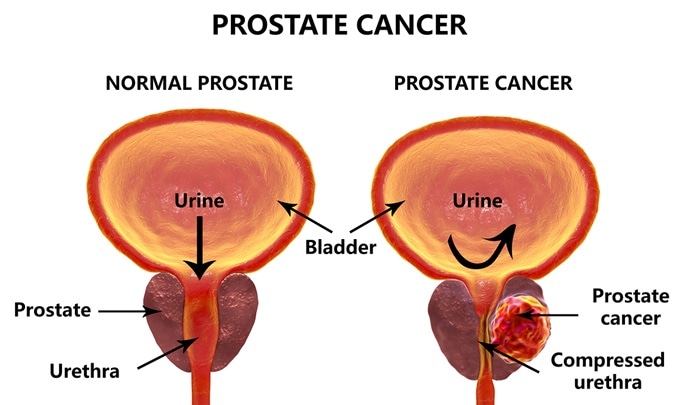
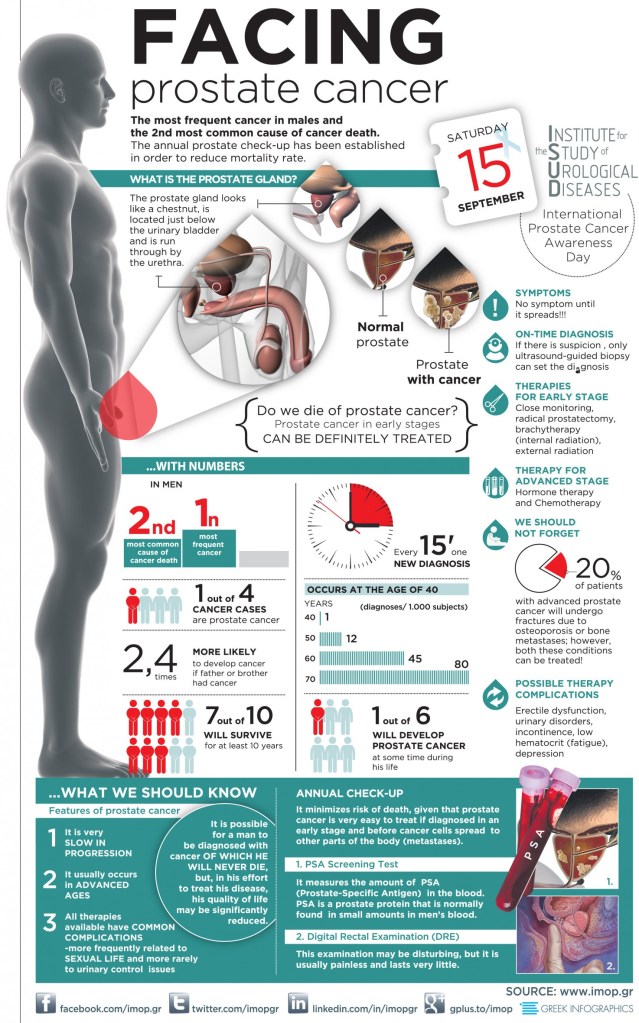
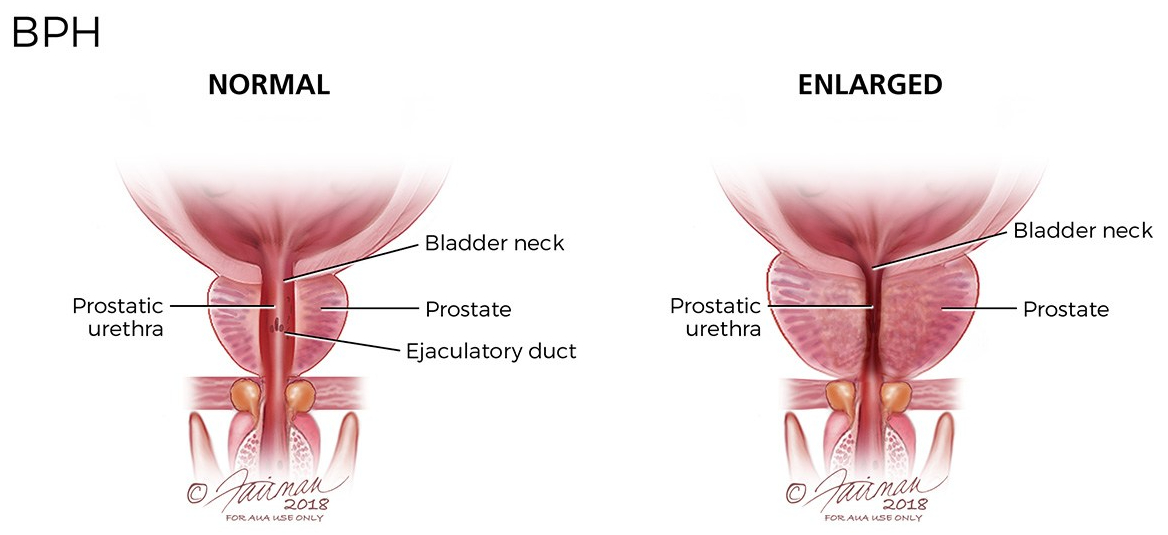
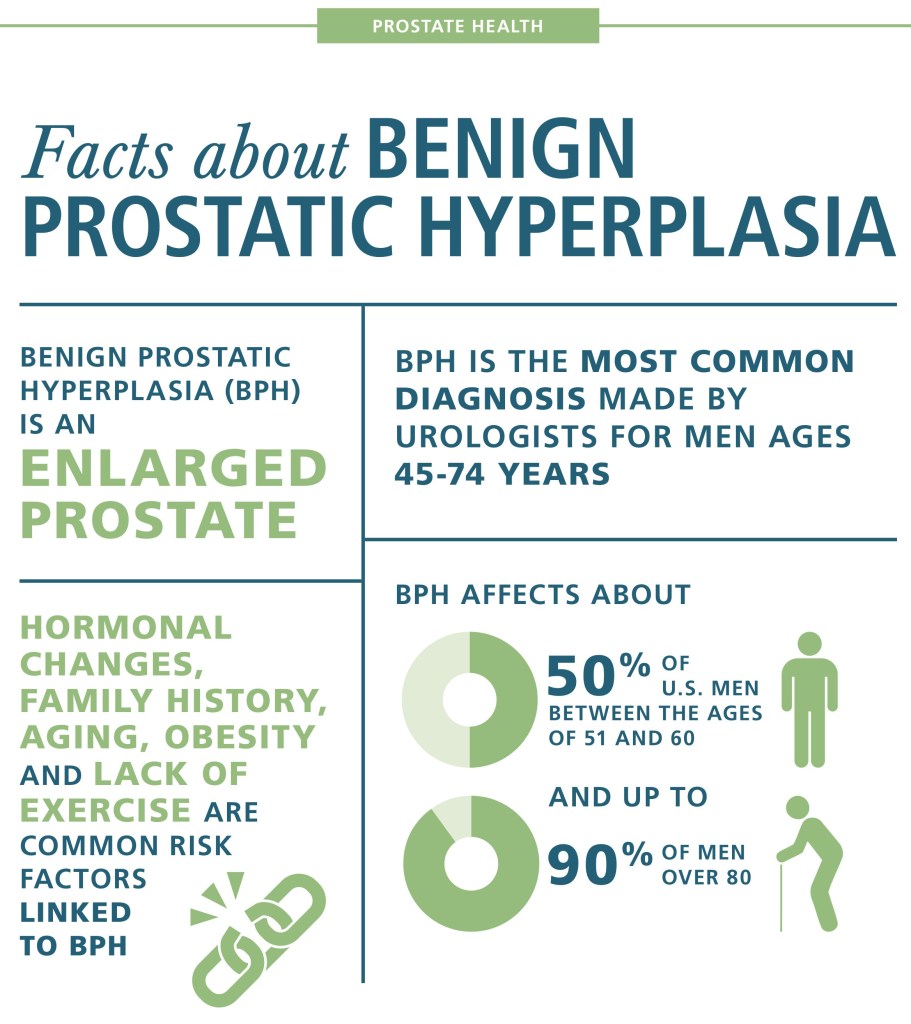
I have known about the Prostate gland, which surrounds the urethral channel exiting the bladder, since med school. I have seen evidence of its enlargement in the increasing time it takes older men to empty their bladders.
When my dad had his prostate surgery, he said that he could blast the porcelain right off the toilet, I could then appreciate for the first time that enlargement of the prostate caused a weak urinary stream.
When I started waking up at night 3 or 4 times to urinate, it really hit home. I had to get something done. My Urologist was a very good one, like all of my doctors. As the old saying goes, the best is none too good when it comes to your health.
On my first visit, he ordered a “Urodynamic” study. In this test, done by a visiting nurse who had the equipment, a small catheter, or tube, ws passed into my bladder, after loading myself with water until I could hold it no longer. The pressure in my bladder was measured, the speed with which I evacuated my bladder was measured, the volume of urine I passed was measured, as well as the volume retained in the bladder.
With these numbers, my bladder volume, residual, and the resistance to flow was calculated. I was shown to have a small bladder, too much residual retained after I emptied it, and an excessive resistance to the flow of urine out of the bladder.
I have not seen the urodynamic studies mentioned in the modern workup of BPH, and it may not have been critically necessary. I did appreciate his thoroughness, however, and factored in the study when he gave me the options of medicine vs. surgery.
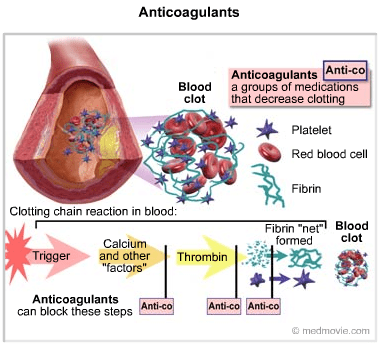
were two medicines mentioned, an alpha adrenergic agonist, and finasteride, an anti-androgen. Since I would have to take both meds the rest of my life, I chose surgical enlargement of the urinary passage through the prostate, known technically as a “roto rooter job”. I, too, noticed the power of my urinary stream after the surgery.
A good friend of mine, also a physician, took medicines for many years, in spite of increasing trouble urinating, getting up at night, and frequent bathroom trips during the day. He eventually went to see a urologist after he had to go to the ER for completely being unable to pass urine.
The Urologist declined to do surgery on the basis of his health, the unusually large size of the blockage, and degree of obstruction. He used a catheter to relieve himself several times a day for the rest of his life. Had I been in his shoes, I would have tried to find a willing surgeon somewhere, perhaps at a university med school.
But then again, I wouldn’t have waited so long. These days many more options are available, and the appended article discusses some of them. –