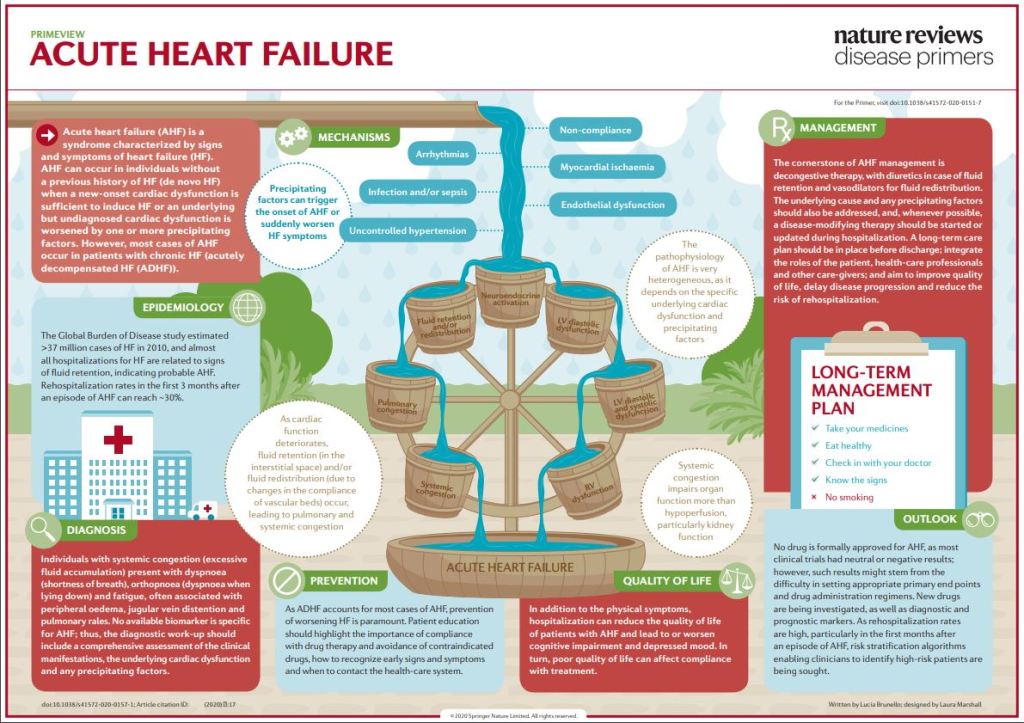
Acute heart failure (AHF) is a syndrome defined as the new onset (de novo heart failure (HF)) or worsening (acutely decompensated heart failure (ADHF)) of symptoms and signs of HF, mostly related to systemic congestion. In the presence of an underlying structural or functional cardiac dysfunction (whether chronic in ADHF or undiagnosed in de novo HF), one or more precipitating factors can induce AHF, although sometimes de novo HF can result directly from the onset of a new cardiac dysfunction, most frequently an acute coronary syndrome.
Despite leading to similar clinical presentations, the underlying cardiac disease and precipitating factors may vary greatly and, therefore, the pathophysiology of AHF is highly heterogeneous. Left ventricular diastolic or systolic dysfunction results in increased preload and afterload, which in turn lead to pulmonary congestion. Fluid retention and redistribution result in systemic congestion, eventually causing organ dysfunction due to hypoperfusion. Current treatment of AHF is mostly symptomatic, centred on decongestive drugs, at best tailored according to the initial haemodynamic status with little regard to the underlying pathophysiological particularities.
As a consequence, AHF is still associated with high mortality and hospital readmission rates. There is an unmet need for increased individualization of in-hospital management, including treatments targeting the causative factors, and continuation of treatment after hospital discharge to improve long-term outcomes.
COMMENTARY:
High frequency sound (ultrasound) bounces off of tissues, like an echo, and allows an electronic look at the heart. Doppler echocardiography is the doctors method of choice for evaluating a heart failure. One of the most important numbers determined by this method is the EJECTION FRACTION, which is a measure of heart efficiency. If the ejection fraction is low, let’s say below 45%, the heart is pumping out only 45% of its volume with each stroke, which means it must work harder to produce the same amount of circulation. The normal is about 60%.
This is the basis of SYSTOLIC Heart failure.
The test can also tell about blood coming into the heart; the early part of the blood entering is usually 80% of the total. If it drops, let’s say below 50%, it means the heart is stiff and resists blood coming in, which is the basis of DIASTOLIC heart failure.
FACES Is an acronym-mnemonic for the symptoms of heart failure. F is for FATIGUE.
A is for ACTIVITY LIMITATION. C is for CONGESTION in the lungs. E is for EDEMA, or swelling, usually of the ankles and legs. S is for SHORTNESS of BREATH.
If you want to remember a bit about heart failure, think about echoes and faces. If your Doctor orders an ultrasound with Doppler, be sure to ask about your ejection fraction and percent of blood that enters early, before the “atrial kick”. Being informed is always a good thing.
To be honest, I have never encountered a person who was given a Doppler echocardiogram and could tell me what his ejection fraction was, but I am eternally hopeful.
—Dr. C.