Warmer weather brings more opportunities for picnics, barbecues and gatherings around food. But before you reach for a second helping, consider if what you’re eating may be increasing your risk for chronic disease. Dr. Ivan Porter II, a nephrologist at Mayo Clinic. Dr. Porter explains dietary changes can have a significant impact on their blood pressure and overall health.
Tag Archives: Chronic Disease
HEALTH: ‘DIABETES AND CHRONIC KIDNEY DISEASE’ – NEW GUIDELINES (OCT 2020)
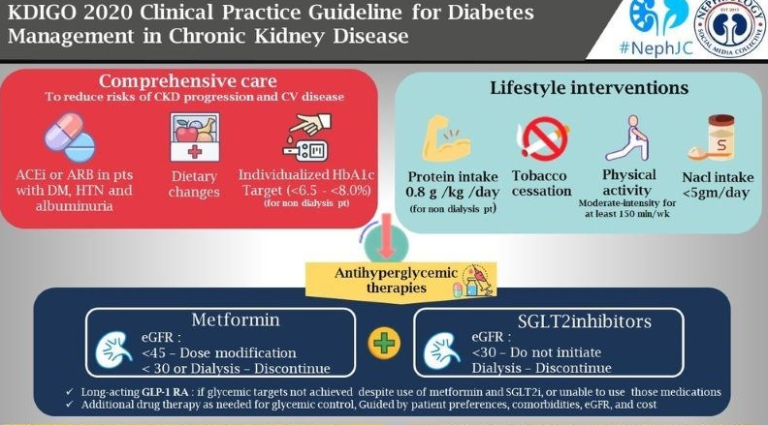

Comprehensive care in patients with diabetes and CKD
Management of CKD in diabetes can be challenging and complex, and a multidisciplinary team should be involved (doctors, nurses, dietitians, educators, etc). Patient participation is important for self-management and to participate in shared decision-making regarding the management plan. (Practice point).
We recommend that treatment with an angiotensin-converting enzyme inhibitor (ACEi) or an angiotensin II receptor blocker (ARB) be initiated in patients with diabetes, hypertension, and albuminuria, and that these medications be titrated to the highest approved dose that is tolerated (1B).
Lifestyle interventions in patients with diabetes and CKD
We suggest maintaining a protein intake of 0.8 g protein/kg)/d for those with diabetes and CKD not treated with dialysis (2C).
On the amount of proteins recommended in these guidelines, they suggest (‘recommend’ becomes a ‘suggest’ at this level of evidence) a very precise intake of 0.8g/kg/d in patients with diabetes and CKD. Lower dietary protein intake has been hypothesized but never proven to reduce glomerular hyperfiltration and slow progression of CKD, however in patients with diabetes, limiting protein intake below 0.8g/kg/d can be translated into a decreased caloric content, significant weight loss and quality of life. Malnutrition from protein and calorie deficit is possible.
Physical activity
We recommend that patients with diabetes and CKD be advised to undertake moderate-intensity physical activity for a cumulative duration of at least 150 minutes per week, or to a level compatible with their cardiovascular and physical tolerance (1D).
VIRTUAL HEALTH: “CHRONIC CARE MANAGEMENT” PROVES VALUE OF TELEMEDICINE
From a ComputerWorld article (April 27, 2020):
“While the pandemic will prove the value of virtual care in a crisis, it will also demonstrate the effectiveness for ongoing chronic care management,” she said. “This moment will have a lasting effect on the adoption of virtual care and accelerate the shift from in-person care to virtual first engagement for multiple conditions and use cases.”

While the need for remote care will not be as acute once the pandemic crisis subsides, demand for telehealth systems will likely remain high. Forrester now expects more than one billion virtual care visits this year, the vast majority of them related to COVID-19.
“…After the crisis subsides, there will be a patient population that will want to continue to receive care online for some things, like managing chronic conditions, follow-up visits after an inpatient stay, surgery or to discuss diagnostic results,” she said.
In this case, it will be important for healthcare providers to ensure that patients are aware of the availability of services.



