Lupus, which used to be called lupus erythematosus because of its butterfly rash and light sensitivity, is an auto immune disease, along with celiac disease and several other autoimmune diseases, it is the great imitator. It can affect almost any organ system.
The great variety of symptoms, and relative rarity leads to a difficulty in establishing the diagnosis. Eventually, you may be lucky enough to find someone who figures it out.
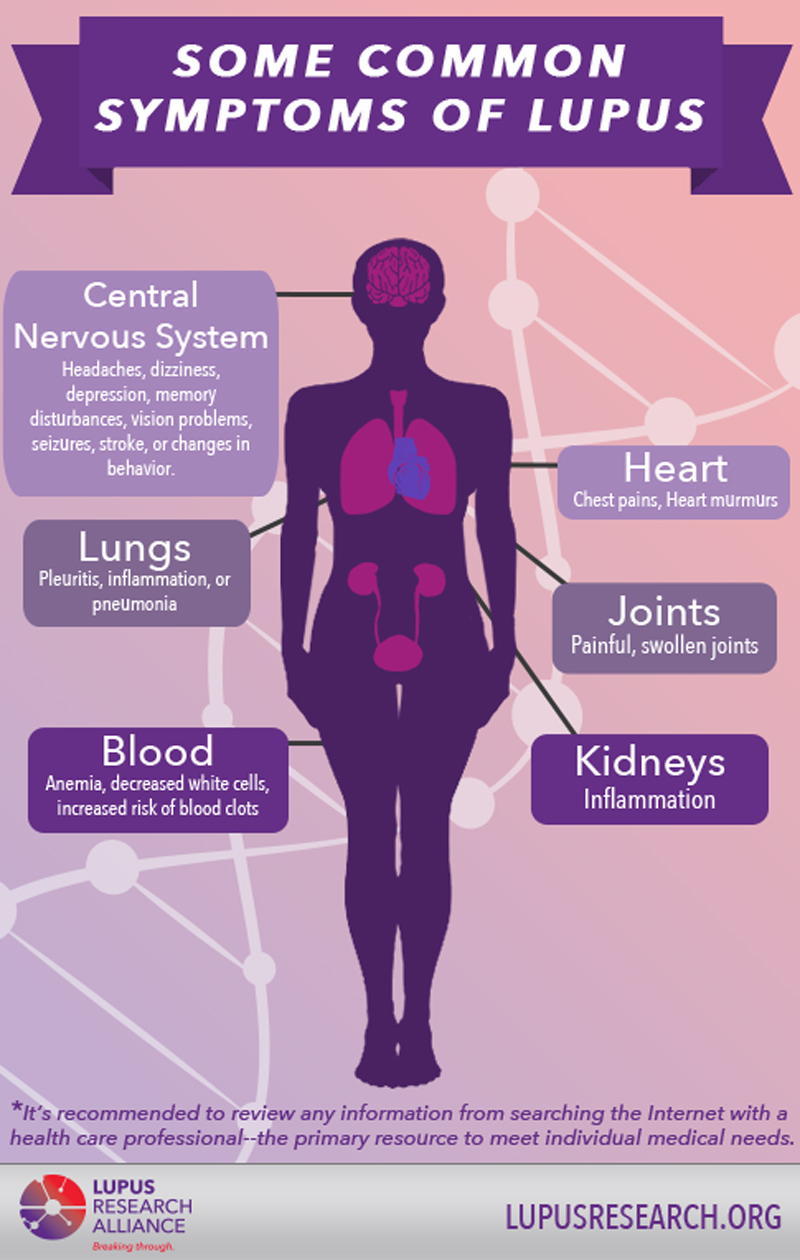
The butterfly rash over the bridge of the nose and cheeks is the most typical finding but it’s not present in all patients. Rheumatoid symptoms, including fatigue fever and joint involvement is common. Chest pain and shortness of breath can occur. Headache confusion and memory loss occurs. Involvement of the kidneys can also occur, it is often the involvement that is life-threatening. These are symptoms maywax and wane over a number of years.
The cause of lupus may involve a black background of infection, the medication, or even sunlight. As with most auto immune diseases, the actual cause is obscure.
Laboratory findings may include an anemia, kidney or liver involvement, and especially anti-nuclear antibody’s. Most people with lupus have a positive ANA test, but not all people with these positive tests have lupus. Other test maybe necessary.
Treatment is usually with Drugs which diminish the immune system. Targeting the B-lymphocytes specifically with rituximab or bulimumab may be helpful.
Lupus, the wolf, can be stealthy and severe. Patients often have to be their own advocate in order to get properly treated.
Please see the following mail clinic article for more information.