JAMA Network (February 2023) – Guillain-Barré syndrome (GBS) is a rare neurological disease that affects the peripheral nerves and causes muscle weakness.
Guillain-Barré syndrome is an autoimmune disease that affects the nerves outside the brain and spinal cord (the peripheral nerves) and develops over several days to weeks. GBS can cause severe muscle weakness, and death occurs in about 5% of patients. The most common subtypes are acute inflammatory demyelinating polyradiculoneuropathy (AIDP) and acute motor axonal neuropathy (AMAN). Approximately 90% of people with GBS in North America and Europe have AIDP.
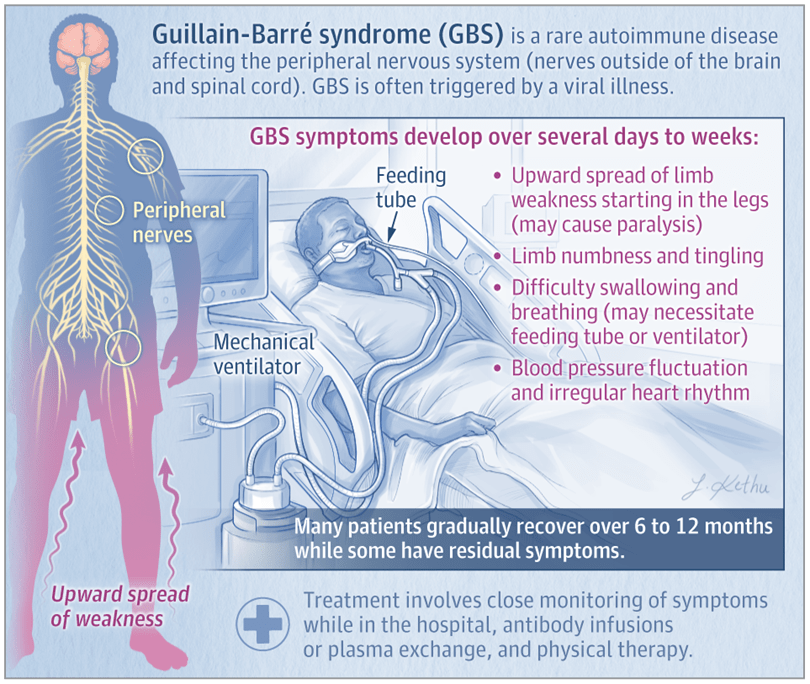
Signs and Symptoms of GBS
Patients with the AIDP subtype of GBS typically have weakness that starts in the legs and spreads to the arms, as well as decreased or absent reflexes. In more than 50% of these patients, nerves that originate in the brain stem (cranial nerves) are affected, which may cause facial weakness, difficulty swallowing, and eye muscle weakness or paralysis. Approximately 25% to 30% of patients develop severe weakness or paralysis of the muscles used to breathe. GBS commonly causes symptoms of low back pain and limb numbness and tingling, and fluctuations in blood pressure or an irregular heart rhythm can also occur.
Risk Factors and Conditions Associated With GBS
GBS affects people worldwide, and the lifetime risk of GBS is estimated at 1 in 1000. Although individuals of any age can develop GBS, the incidence increases with age, and males are slightly more likely to develop GBS than females.
Approximately two-thirds of patients have a diarrheal or respiratory illness within 4 to 6 weeks prior to the onset of GBS symptoms. Other, less common events or conditions that may trigger GBS include recent surgery, pregnancy, and immunosuppression. Although rare sporadic cases of GBS have been reported after vaccinations, the risk of developing postvaccination GBS is much lower than the risk of developing GBS after an infection.
Diagnosis and Treatment of GBS
Diagnosis of GBS is made based on symptoms and physical examination findings. Neurological testing often includes electromyography and nerve conduction studies to assess nerve and muscle function. Results of a spinal tap (lumbar puncture) may support the diagnosis of GBS and can rule out other neurological diseases.
Individuals with suspected GBS should be admitted to the hospital. All patients with GBS need close monitoring of their breathing, heart rate, and blood pressure. Individuals who develop severe respiratory muscle weakness or paralysis are supported with mechanical ventilation. Patients who have difficulty swallowing may receive nutrition through a feeding tube.
Current recommended treatments for GBS are intravenous immune globulin (IVIG), an infusion of antibodies, or plasma exchange, which involves removal and replacement of the liquid component of blood. About 40% to 50% of patients with GBS do not improve within 4 weeks after IVIG or plasma exchange and need prolonged supportive care. Physical, occupational, and speech therapy are important to help patients regain strength and function.
What Is the Prognosis of GBS?
Most patients with GBS gradually improve and can have a complete recovery over 6 to 12 months. However, some patients have residual symptoms, including fatigue, pain, numbness, tingling, and muscle weakness. Some factors associated with a higher risk of death due to GBS include older age, more severe disease, and need for mechanical ventilation.


