You should get your flu shot this year. Not only has he influenza Genie been kept in its bottle by Covid precautions, and overdue for a bad year, but the H3N2 serotype circulating around is a good match for today’s vaccine; you may have been disappointed by the lack of protection in the past, due to the vaccine poorly matching the prevalent infecting serotype, caused by the rapid change of the virus and slow changes in the vaccine.
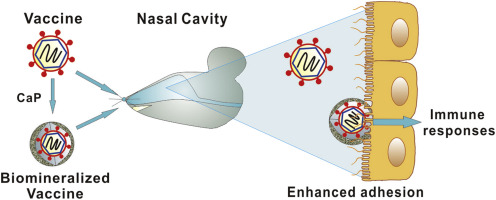
With RSV already making a comeback, influenza likely to be bad, and Covid likely a big problem also, You would be well advised to start going back to your masks, keeping your distance, avoiding large groups, and making sure your inside exposures are well ventilated, not to mention getting the most recent covalent Covid shot, which contains BA.1 and BA.2.
The common cold with running nose, sneezing, and nasal congestion, is usually caused by rhinoviruses, of which there are several hundred serotypes, although can be caused by any of the respiratory viruses. Whenever I traveled, I often came back with a cold because my immunity at home was based on the common rhinoviruses at home, and when I traveled, I encountered different types, to which I was not immune. Many other viral types can also cause the common cold including influenza, para influenza, and even coronavirus. In asthmatic children, the rhinovirus also produces an asthmatic response, often severe.
Croup in children is often produced by parainfluenza type one virus.
Bronchiolitis in children is usually caused by RSV. There is currently no vaccine for RSV.
Influenza, the “flu”, starts out with chills and fever, often settles into the lung. The influenza virus is usually the initiating culprit, but bacterial infection often follows. Coronavirus infection may start as “the flu” with the respiratory symptoms, such as runny nose, sore throat, and cough following.
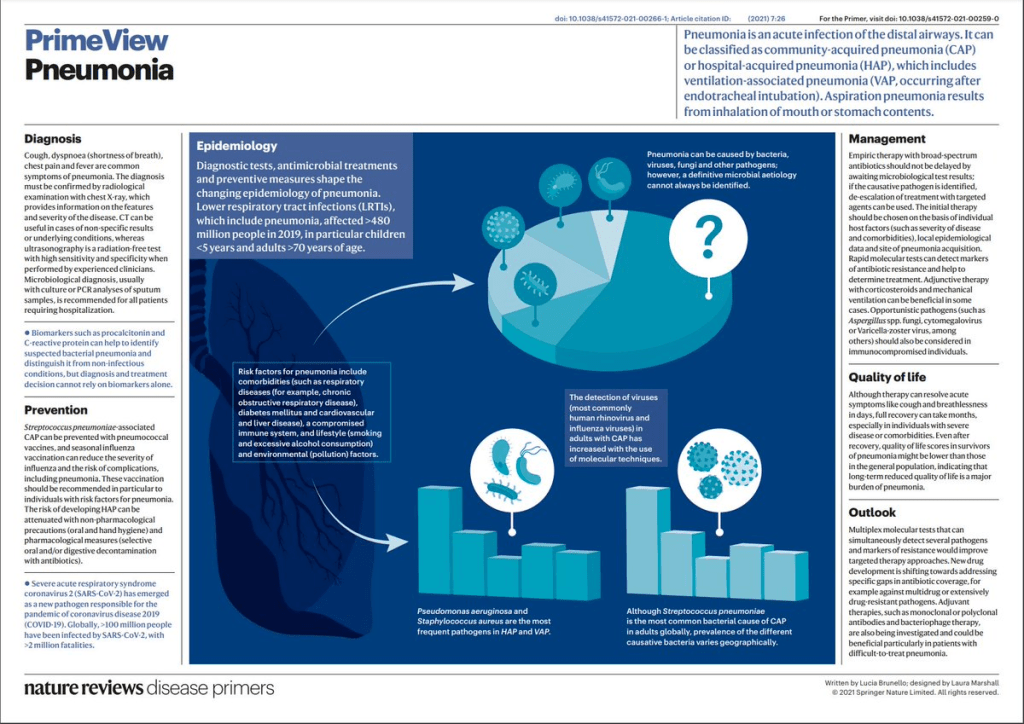
Pneumonia is often produced by coronavirus, Especially the early strains. The more recent epidemic strains such as BA .1, Seem to have traded increased transmissibility for less lung affinity.
Avian influenza, H5N1 Is highly lethal with pneumonia, but you catch it from birds rather than people at the present time. Watch out if it ever starts spreading from human to human.
Most respiratory infections begin as a viral infection, which are not affected by antibiotics. Bacterial complications, such as otitis media, sinusitis, and pneumonia may follow, facilitated by the viruses, which lower immune resistance.
There are a number of antiviral agents, especially for coronavirus and Influenza. RSV may have effective treatments, which are needed particularly in babies.
–Dr. C