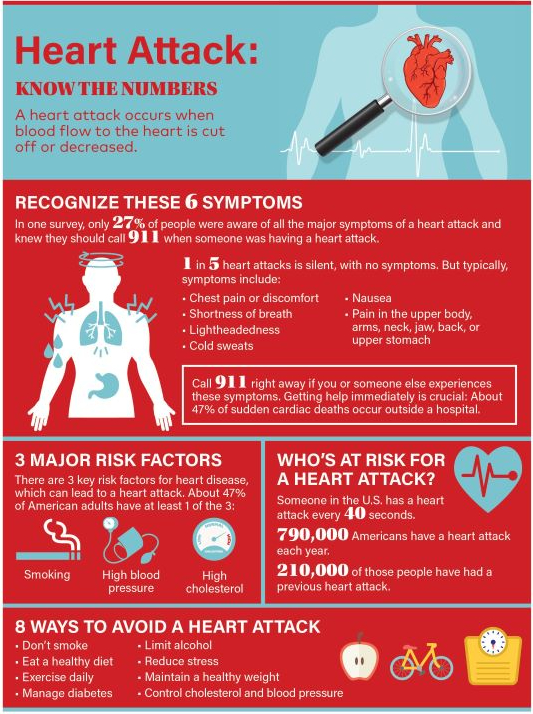
Heart attacks are something that most people know about; the sudden severe chest pain, radiating into the jaw or left arm, associated with shortness of breath, nausea, and the like. However there’s a lot of confusion also; not all heart attacks have typical symptoms (silent heart attacks). Some significant chest pain is not due to a heart attack, and some significant cardiac disease is something different from a heart attack.
I will cover these three scenarios one at a time, beginning with the most dangerous, the silent heart attack.
The silent heart attack has the same effect as the more typical variety, and is caused by blockage in the coronary arteries, which interferes with oxygen and glucose delivery, and causes death of heart muscle. It occurs under physically or emotionally stressful circumstances, particularly in the cold. It may be more common in women, and accounts for at least half of all heart attacks.
Risk factors are identical to those of a regular heart attack, and include being overweight, diabetic, not exercising regularly, having high blood pressure, high cholesterol or smoking cigarettes.
The symptoms may be Flu like, fatigue, indigestion, and perhaps a soreness in the chest, upper back, arms or jaw. My mother-in-law died in my house after a stressful incident, and was heard to be vomiting in the middle of the night. My father had inordinate fatigue and paleness, which caused my mother to take him to the doctor, who sent him by ambulance for a bypass operation.
Many silent heart attacks are discovered when the doctor takes an electrocardiogram in the course of an examination. This is a good argument for the regular physical examination, since having a silent heart attack increases the likelihood that you will have another.
The frequency and seriousness of heart attacks is of course an excellent argument for proper sleep, diet, exercise, and other good preventative habits.
—Dr. C.



