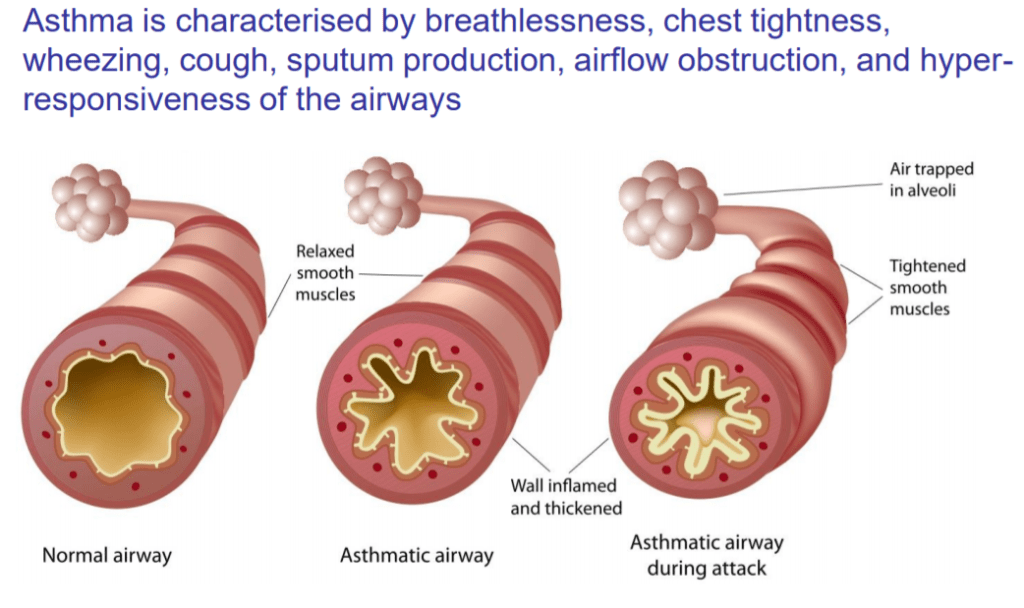
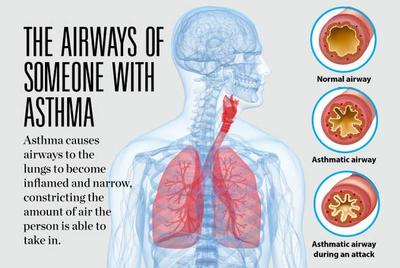
Asthma is a lung condition with narrowing of the airways, especially on exhalation, or breathing out. This narrowing leads to the musical sound on breathing the air out of the lungs that I heard so often with my stethoscope and over the phone, when I was in active allergy practice. With an asthma attack, the blockage to airflow can become severe enough to dangerously raise the carbon dioxide concentration in the blood stream, and lower the oxygen content.
Many attacks occurred at night .Over the phone, I had older kids and adults take a deep breath, and count from 1 to 30 as rapidly as they could. If they could count out loud to 30 with one breath, at least the obstruction and attendant blood gas changes were not usually serious at that moment in time. That helped me decide whether or not I had to see them in the emergency room.
Asthma is an inflammatory condition of the lining of the airway that stimulates the smooth muscle surrounding the airway to constrict and obstruct flow of air, particularly on exhalation. Early on in my medical practice the main pathology was thought to be overactive airway muscles, and the main effort was to relax those muscles so that breathing could be easier. This was typically done with adrenaline injections, or the inhalation of adrenaline-like agents such as albuterol.
More sustained opening the airway was accomplished by oral theophylline. As time went on, it became known that its effectiveness required a certain blood level. We had an HPLC machine in the office to measure this. 5 to 10 µg per milliliter was required for relief, and anything over 20 µg per milliliter was dangerous. Many cases of convulsions have been recorded in people with excessive blood levels.
We were always aware of the fact that cortisone medications would relieve asthma, but regular use of these drugs caused worrisome side effects such as interference with growth in children, osteoporosis, weight gain and loss of sleep or other problems. Most worrisome was the possibility of adrenal insufficiency and sudden death. We used Cortisone only as a last resort.
There was a group of young children especially 1 to 6 years of age that developed extreme asthma a few days after they developed a common cold. I found that giving prednisolone for two or three days at the start of a runny nose would block the advent of this asthma, without suppressing the adrenal gland. Three days of prednisone was also used to blunt severe attacks.
The excellence of Cortisone in the treatment of asthma should’ve told us that inflammation was a particularly important factor. It is now known that Asthma is not a disease of airway smooth muscle sensitivity per se, but rather a chronic inflammation of the airways that causes the muscles to be irritable.
Asthma is more common in allergic individuals, particularly when they are young. For this reason, the allergies are treated by avoidance of exposure to such things as cats, dogs, house dust and pollen. Allergy injections to the skin test positive items is also useful.
Currently, asthma is treated by inhaling special cortisone preparations and long acting bronchodilators.
The chain of chemical reactions that cause asthmatic airway inflammation has become apparent over the years. Drugs to block these are available, and include special antibodies can be exceptionally expensive; but very effective.
The youngest of my former partners is still practicing Allergy, and almost never has to deal with acute severe asthma.
The beast has been tamed, if not conquered.