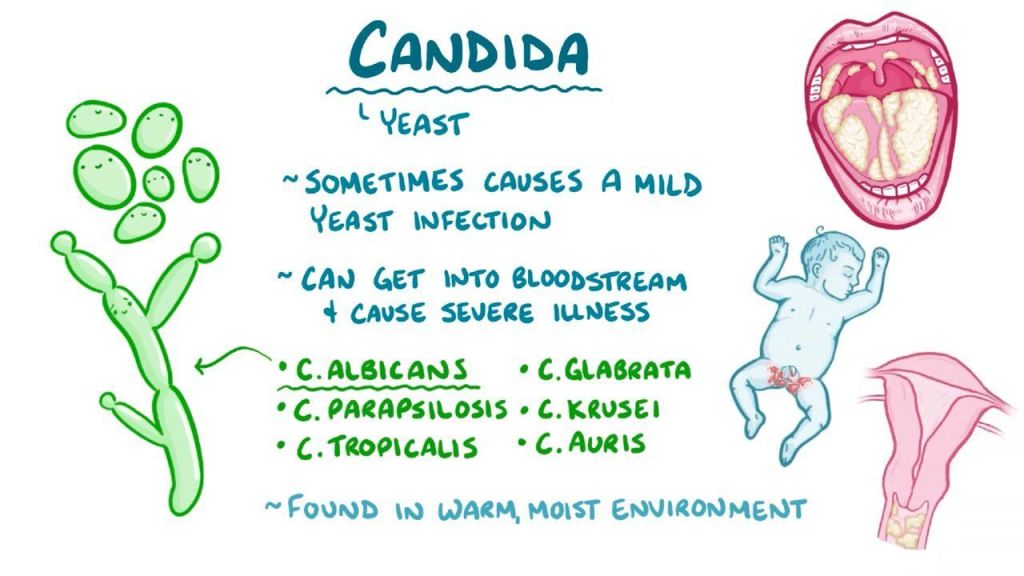
Candida auris is a type of fungus, a yeast in this case, that is increasing in frequency and spreading geographically, apparently due to warmer temperatures. This organism is fairly common in hospitals, where it often is on the skin. It is lethal if it gets into the body, and often difficult to treat. Las Vegas, Nevada, in particular is having almost an epidemic of these infections, with more than 500 infections and 100 deaths since the fall of 2021.

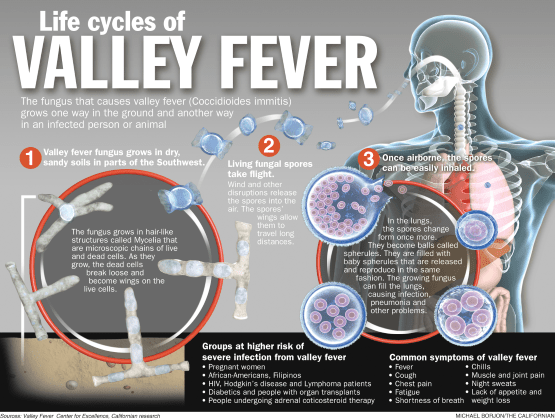
An alarming number of cases are misdiagnosed when patients first come to the emergency room; fungal infection is certainly not the first thing a doctor thinks of when she sees a patient with a febrile illness. On the flipside of that, any delay in diagnosis, particularly with a bloodstream infection, can be lethal. There are a few good laboratory tests for the diagnosis of fungal infection, and many of these take highly trained technicians with a microscope.
Fungi are opportunistic infections, which means a healthy person is unlikely to be seriously affected. With cancer treatments and organ transplants, increasing numbers of people are on immunosuppressive drugs which means they are more susceptible. Hospitals deal with this very sick people, and frequently use central catheters inserted into patients veins, and opportunistic fungi, like candida auris, get a free ride into the body. With fever, most doctors, think first of bacterial infections, and give antibiotics; these antibiotics can actually worsen fungal infection, since they remove bacterial competitors.
Many medical schools do not teach their students about fungal infections, and in 4 years of medical school, doctors in training are lucky to get two or three hours on this subject. Fungal infections are thought to be rare.
In these days of high-tech, corporate medicine, it is good for a patient to be her own advocate. Don’t be afraid to ask the doctor if she has thought of fungal infection as possible cause if you are not improving with your treatment, particularly if you’re in the hospital.
—Dr. C.